Pyridoxine-dependent seizure (PDE) is a rare, autosomal recessive genetic disorder characterized by recurrent seizures that are unresponsive to conventional antiepileptic medications but dramatically responsive to pyridoxine (vitamin B6) supplementation. PDE usually manifests in neonates or infants and, without prompt recognition and treatment, can lead to significant neurodevelopmental impairment.
Pathophysiology and Genetic Basis of Pyridoxine-Dependent Seizure
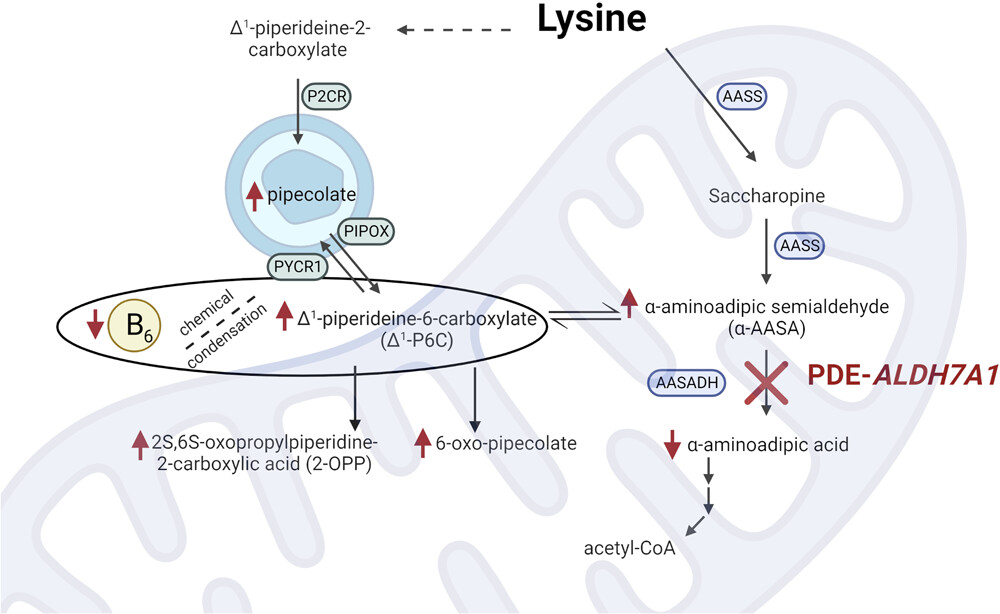
PDE results from mutations primarily in the ALDH7A1 gene, which encodes antiquitin, a crucial enzyme involved in lysine metabolism. The deficiency of antiquitin leads to the accumulation of metabolites that bind and inactivate pyridoxal 5’-phosphate (PLP), the active form of vitamin B6 essential for neurotransmitter synthesis. This biochemical disruption results in neuronal hyperexcitability and seizures.
Genetic Mutations Associated with PDE
- ALDH7A1 gene mutations: Most common cause
- PLPBP gene mutations: Associated with a variant form of PDE
- PNPO deficiency: May present with overlapping features
Timely genetic testing is critical for a definitive diagnosis and genetic counseling.
Clinical Presentation of Pyridoxine-Dependent Seizures
Neonatal Period
- Seizures within hours to days after birth
- Seizure types include generalized tonic-clonic, myoclonic, and focal seizures
- Poor feeding and irritability
- Hypotonia and apnea
Infancy and Later
- Developmental delay
- Cognitive impairment if untreated
- Behavioral disturbances
Atypical cases may present later in infancy or even childhood, often leading to delayed diagnosis.
Diagnostic Approach to Pyridoxine-Dependent Seizure
Clinical Evaluation
Early suspicion is crucial in neonates presenting with refractory seizures unresponsive to standard antiepileptic therapy.
Biochemical Testing
- Measurement of urinary biomarkers: Elevated α-aminoadipic semialdehyde (AASA) and pipecolic acid
- Plasma and CSF analysis: Decreased PLP levels
Genetic Testing
Definitive diagnosis is achieved through molecular genetic testing of the ALDH7A1 gene.
Pyridoxine Trial
Administering intravenous pyridoxine (100 mg) under EEG monitoring can lead to abrupt seizure cessation, confirming the diagnosis in emergent situations.
Management of Pyridoxine-Dependent Seizure
Acute Treatment
- Initial Pyridoxine Dose: Administer 100 mg IV slowly under EEG monitoring to avoid respiratory depression
- Seizure Control: Rapid resolution of seizures typically occurs within minutes
Long-Term Treatment
- Maintenance Therapy: Oral pyridoxine at a dose of 30–100 mg/day
- Monitoring: Regular EEGs and developmental assessments
- Adjunctive Therapy: Some patients benefit from lysine-restricted diets and arginine supplementation to reduce toxic metabolite accumulation.
Special Considerations
- Prenatal Treatment: In cases of a known family history, maternal supplementation during pregnancy can prevent neonatal seizures.
- Neurodevelopmental Support: Early intervention therapies to address potential cognitive and motor deficits.
Prognosis of Pyridoxine-Dependent Seizure
With early diagnosis and appropriate pyridoxine supplementation, many children achieve seizure control and improved developmental outcomes. However, some patients may still experience learning disabilities or behavioral issues, especially if diagnosis and treatment are delayed.
Prognosis is significantly enhanced by:
- Early initiation of therapy
- Adequate pyridoxine dosing
- Comprehensive neurodevelopmental support
Differentiating Pyridoxine-Dependent Seizure from Related Disorders
Pyridoxine-Responsive Epilepsy
Not genetically linked to ALDH7A1 mutations but responds to vitamin B6; generally has a better prognosis.
Pyridox(am)ine 5′-Phosphate Oxidase (PNPO) Deficiency
Requires treatment with PLP instead of pyridoxine and may present with similar neonatal seizures.
Recognizing these differences is essential to selecting the appropriate therapeutic strategy.
Frequently Asked Questions
What triggers pyridoxine-dependent seizures?
PDE is genetically triggered by mutations affecting vitamin B6 metabolism, not by external triggers.
How is pyridoxine-dependent seizure diagnosed?
Diagnosis relies on clinical suspicion, biochemical markers, a trial of pyridoxine, and genetic testing.
Can pyridoxine-dependent seizures be prevented?
Prenatal supplementation in at-risk pregnancies can prevent neonatal seizure onset.
Is lifelong pyridoxine therapy necessary?
Yes, individuals with PDE require lifelong vitamin B6 supplementation to maintain seizure control.
What is the outcome for children treated early for PDE?
Children diagnosed and treated early often achieve good seizure control and improved developmental outcomes, though some may have residual learning challenges.