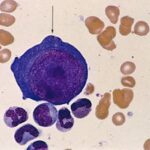
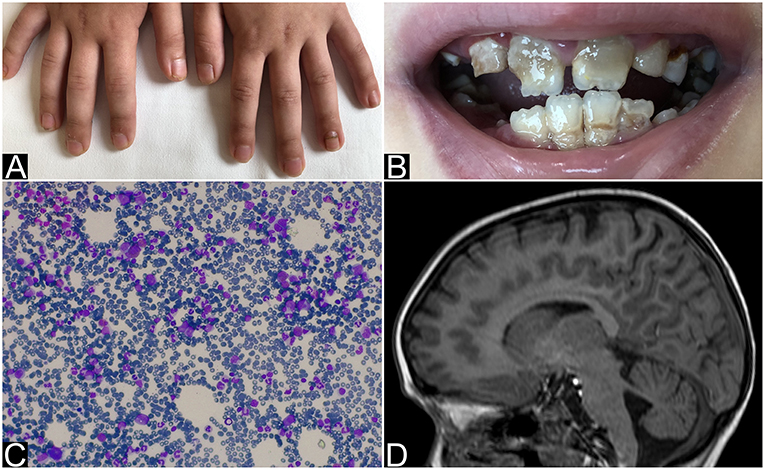
Pure red cell aplasia (PRCA) is a rare hematologic syndrome characterized by severe normocytic anemia, reticulocytopenia, and selective absence of erythroid precursors in the bone marrow. Chronic lymphocytic leukemia (CLL), a common B-cell lymphoproliferative disorder in adults, is frequently associated with autoimmune complications. Among these, PRCA represents a serious but uncommon manifestation, likely resulting from immune dysregulation inherent to CLL.
Timely identification of PRCA in CLL patients is essential for prompt intervention, preventing complications from persistent anemia, and guiding individualized treatment decisions.
Pathophysiology: Immune-Mediated Erythropoietic Suppression in CLL
In the context of CLL, PRCA arises from a disrupted immune environment that targets erythroid progenitor cells. The pathogenic mechanisms include:
- T-cell Dysregulation: Autoreactive cytotoxic T lymphocytes destroy erythroid precursors.
- B-cell Dysfunction: Monoclonal B cells produce autoantibodies that neutralize erythropoietin or target erythroid cells directly.
- Immune Complex Deposition: Circulating immune complexes may impair erythropoiesis.
The immunologic imbalance in CLL—marked by hypogammaglobulinemia, abnormal cytokine profiles, and altered regulatory T-cell activity—contributes significantly to PRCA pathogenesis.
Clinical Presentation: Recognizing PRCA in CLL Patients
The symptomatology of PRCA in CLL is often masked by features of the underlying leukemia. Nevertheless, isolated anemia with absent reticulocytosis should prompt suspicion.
Common Features:
- Fatigue, pallor, dyspnea
- Absence of bleeding or infections typical of pancytopenia
- Stable white cell and platelet counts
- Progressive or refractory anemia during CLL treatment
Diagnostic Evaluation: Confirming PRCA in the CLL Setting
A structured diagnostic pathway is vital for accurate identification of PRCA in patients with CLL. It entails exclusion of alternative anemia causes and verification of erythroid aplasia.
Differential Diagnosis
It is imperative to distinguish PRCA from other hematologic and non-hematologic causes of anemia in CLL:
| Differential | Distinguishing Feature |
|---|---|
| Autoimmune Hemolytic Anemia | Elevated LDH, indirect bilirubin, spherocytes |
| Marrow Infiltration | Pancytopenia, leukoerythroblastosis |
| Aplastic Anemia | Global marrow hypoplasia |
| Anemia of Chronic Disease | Mild anemia, normal reticulocyte count |
| Myelodysplastic Syndrome | Dysplastic changes in marrow, cytogenetic abnormalities |
Management Strategies: Tailoring Treatment for PRCA in CLL
Therapeutic decisions depend on the severity of PRCA, CLL disease status, and response to prior treatments. Goals include restoration of erythropoiesis and control of underlying CLL-driven immune dysfunction.
First-Line Approaches
- Immunosuppressive Therapy:
- Cyclosporine A is highly effective in immune-mediated PRCA.
- Corticosteroids may be used alone or in combination.
- IV Immunoglobulin (IVIG):
Beneficial for patients with parvovirus B19-related PRCA or in those with hypogammaglobulinemia. - Anti-CD20 Therapy (Rituximab):
Targets B-cell clones contributing to autoimmunity. Effective in steroid-refractory cases. - Erythropoiesis-Stimulating Agents (ESAs):
May provide temporary relief but are less effective without resolving the underlying immune suppression.
CLL-Directed Therapy
In cases where PRCA is refractory to immunosuppression or when CLL is active, disease-directed therapies should be considered:
- Ibrutinib, Venetoclax, or Bendamustine-Rituximab (BR) regimens may reduce autoimmune complications by controlling the malignant clone.
Supportive Care
- Red blood cell transfusions for symptomatic anemia
- Iron chelation if transfusion-dependent
- Monitor for infections due to immunosuppression
Prognosis and Long-Term Outcomes
The prognosis of PRCA associated with CLL varies depending on the response to immunosuppressive and anti-leukemic therapies. Patients achieving remission of PRCA typically demonstrate durable responses, particularly with combined immunosuppressive and CLL-specific treatment.
Regular follow-up with complete blood counts, reticulocyte monitoring, and reassessment of marrow status is recommended to evaluate treatment efficacy and detect relapse.
Pure red cell aplasia represents a significant but manageable autoimmune complication in patients with chronic lymphocytic leukemia. Understanding its pathophysiology, ensuring early diagnosis through targeted evaluation, and instituting prompt, individualized treatment strategies are crucial for optimizing patient outcomes. Integration of CLL-directed therapies with immunomodulation offers the best prospects for remission and improved quality of life.