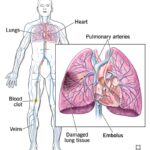
Pulmonary thromboembolism (PTE), a manifestation of venous thromboembolism (VTE), is a preventable but often fatal condition resulting from the obstruction of the pulmonary arteries by thrombotic material. Prevention strategies must be rigorously implemented, particularly in hospitalized and high-risk patients, to reduce morbidity, mortality, and healthcare burden.
Identifying Risk Factors for Pulmonary Thromboembolism
Effective prevention begins with a clear understanding of the contributing risk factors. These can be stratified into patient-related and situational categories.
Patient-Related Risk Factors
- Previous VTE episodes
- Inherited thrombophilia (Factor V Leiden, Protein C/S deficiency)
- Malignancy
- Obesity
- Advanced age
- Chronic heart or respiratory disease
Situational Risk Factors
- Major surgery, especially orthopedic or pelvic
- Prolonged immobility or bed rest
- Trauma
- Pregnancy and postpartum state
- Hormonal therapy or oral contraceptives
- Long-distance travel (economy class syndrome)
Clinical Risk Stratification Tools
Accurate risk assessment allows clinicians to balance the benefits and risks of prophylaxis.
Commonly Used Models
- Caprini Score: Widely used for surgical patients
- Padua Prediction Score: Applied in medical inpatients
- Wells Score: Useful in assessing pretest probability of DVT/PE
Risk Categories
- Low risk: Early ambulation usually sufficient
- Moderate risk: Requires pharmacologic or mechanical prophylaxis
- High risk: Needs combined mechanical and pharmacologic methods
Mechanical Prophylaxis Measures
Mechanical interventions are non-invasive and particularly useful in patients with contraindications to anticoagulants.
Graduated Compression Stockings (GCS)
- Enhance venous return in the lower extremities
- Reduce venous stasis, especially in postoperative patients
Intermittent Pneumatic Compression (IPC) Devices
- Provide cyclical compression to promote blood flow
- Effective in orthopedic surgeries and critically ill patients
Venous Foot Pumps
- Useful for patients unable to tolerate thigh or calf compression
Pharmacologic Prophylaxis Options
Anticoagulants are the cornerstone of PTE prevention in moderate-to-high-risk patients.
Low Molecular Weight Heparin (LMWH)
- Once-daily dosing with predictable pharmacokinetics
- Preferred in most inpatient settings
Unfractionated Heparin (UFH)
- Shorter half-life and reversible with protamine sulfate
- Recommended in patients with renal insufficiency
Direct Oral Anticoagulants (DOACs)
- Include rivaroxaban, apixaban, dabigatran
- Approved for use in postoperative VTE prophylaxis in orthopedic surgeries
Fondaparinux
- Synthetic pentasaccharide with once-daily subcutaneous administration
- Contraindicated in patients with severe renal dysfunction
Special Considerations in Surgical Patients
PTE prevention protocols must be individualized based on the type of surgery and patient-specific factors.
Orthopedic Surgery
- Total hip and knee replacements carry high thrombotic risk
- Extended prophylaxis for up to 35 days is recommended
General Surgery
- Anticoagulation combined with early ambulation is the standard approach
Neurosurgical and Spinal Procedures
- Mechanical methods preferred initially due to bleeding risk
- Transition to anticoagulants when safe
Preventive Strategies in Medical Inpatients
Medical inpatients often have multiple risk factors for thromboembolism, including immobility, infections, and heart failure.
- Use of the Padua Prediction Score to determine need for prophylaxis
- Encourage frequent mobilization and hydration
- Monitor for bleeding risks during pharmacologic therapy
Long-Term PTE Prevention and Outpatient Considerations
Some patients may require continued preventive measures following hospital discharge.
Extended Prophylaxis
- Especially in cancer patients and those with previous VTE
- Use of DOACs for extended periods shown to reduce recurrence
Lifestyle Modifications
- Weight loss in obese individuals
- Smoking cessation
- Increased physical activity and leg exercises during long travel
Patient Education
- Awareness of DVT symptoms: swelling, pain, redness in limbs
- Compliance with medications
- Safe practices during long flights: walking, hydration, leg stretches
Preventing Pulmonary Embolism in Pregnancy
Pregnancy induces a hypercoagulable state, making women more susceptible to thromboembolism.
- Prophylactic LMWH in women with previous VTE or thrombophilia
- Mechanical methods preferred during delivery and postpartum period
- Avoid DOACs due to lack of safety data in pregnancy
Prevention of PTE in COVID-19 Patients
SARS-CoV-2 infection is associated with increased thrombotic complications due to endothelial injury and hypercoagulability.
- All hospitalized COVID-19 patients should receive prophylactic anticoagulation unless contraindicated
- Higher doses may be warranted in critically ill patients
- Monitor for bleeding, renal function, and D-dimer levels
Monitoring and Quality Improvement in PTE Prevention
Hospitals should establish systems to audit compliance with thromboprophylaxis guidelines.
Institutional Protocols
- Standardize risk assessment at admission
- Automated reminders in electronic health records
- Multidisciplinary involvement in prophylaxis programs
Outcome Measurement
- Track incidence of hospital-acquired thromboembolism
- Monitor bleeding rates and adverse drug events
Pulmonary thromboembolism prevention requires a structured, evidence-based approach that includes patient risk stratification, mechanical and pharmacologic prophylaxis, and continuous monitoring. Institutional adherence to established protocols and individualized patient care are essential to mitigating the risk of this preventable condition.