Pulmonary emphysema is a serious and progressive lung condition characterized by the destruction of alveolar walls, leading to reduced oxygen exchange and difficulty breathing. While most cases of emphysema are linked to smoking and environmental factors, a specific genetic condition known as alpha-1-proteinase inhibitor deficiency (alpha-1 antitrypsin deficiency) plays a crucial role in the development of emphysema in a subset of patients. Understanding this genetic link is essential for proper diagnosis, treatment, and management of this form of emphysema.
What is Alpha-1-Proteinase Inhibitor Deficiency?
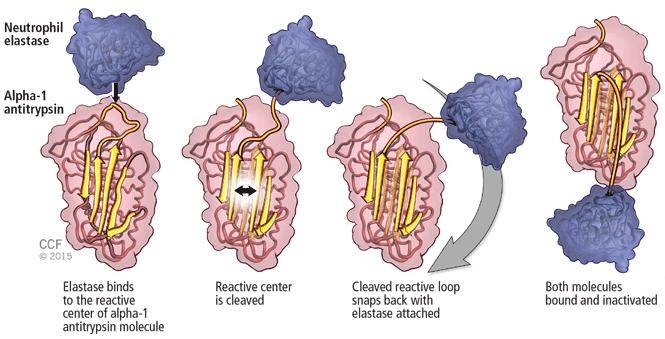
Alpha-1-proteinase inhibitor (A1PI), also known as alpha-1 antitrypsin (AAT), is a crucial enzyme produced by the liver. Its primary function is to protect the lungs from the destructive effects of neutrophil elastase, an enzyme released by white blood cells that can break down lung tissue. A deficiency of A1PI allows neutrophil elastase to damage lung tissues, leading to conditions such as emphysema.
Genetic Causes of Alpha-1-Proteinase Inhibitor Deficiency
Alpha-1-proteinase inhibitor deficiency is an inherited genetic disorder. It results from mutations in the SERPINA1 gene, which provides instructions for producing A1PI. The deficiency is autosomal codominant, meaning that an individual inherits one defective gene from each parent to develop severe symptoms. Individuals who inherit only one defective gene (heterozygotes) may have mild symptoms or none at all but can still pass the condition on to their children.
How Alpha-1-Proteinase Inhibitor Deficiency Causes Emphysema
The deficiency of alpha-1-proteinase inhibitor allows the unchecked activity of neutrophil elastase in the lungs. This leads to the destruction of alveolar walls, where gas exchange occurs. Over time, the damage causes the air sacs to enlarge and lose their elasticity, reducing the lungs’ ability to expel air and leading to the symptoms of emphysema.
The Role of Neutrophil Elastase in Lung Damage
Neutrophil elastase is an enzyme responsible for breaking down proteins in the lungs as part of the body’s immune response. In individuals with A1PI deficiency, the inability to neutralize this enzyme results in the degradation of the alveolar walls and the destruction of lung tissue. This process worsens as the individual ages, leading to progressive lung damage.
Symptoms of Pulmonary Emphysema Associated with Alpha-1-Proteinase Inhibitor Deficiency
The symptoms of emphysema related to alpha-1-proteinase inhibitor deficiency are similar to those of other types of emphysema but tend to manifest earlier in life. Individuals with this condition may experience:
1. Shortness of Breath (Dyspnea)
As lung function deteriorates, individuals may experience increasing difficulty with breathing, particularly during physical exertion. This symptom worsens as the disease progresses.
2. Chronic Cough and Sputum Production
Chronic cough with mucus production is common in patients with emphysema due to alpha-1-proteinase inhibitor deficiency. The body attempts to clear the airways of the mucus that accumulates as a result of the damage to the lung tissues.
3. Wheezing
Wheezing, or a high-pitched whistling sound when breathing, can occur due to airway narrowing. This is often observed when the lungs are unable to expel air fully during exhalation.
4. Fatigue
As the lungs become less efficient at exchanging gases, individuals may feel fatigued and unable to perform normal daily activities. This results from reduced oxygen supply to the body.
5. Cyanosis
In advanced stages, low oxygen levels in the blood can cause a bluish color to appear in the skin, especially around the lips and fingertips, a condition known as cyanosis.
Diagnosis of Pulmonary Emphysema Associated with Alpha-1-Proteinase Inhibitor Deficiency
Diagnosing emphysema associated with alpha-1-proteinase inhibitor deficiency requires a combination of clinical evaluation, genetic testing, and specialized lung function tests. Some of the most common diagnostic methods include:
1. Medical History and Physical Examination
A thorough medical history and physical exam are critical. The healthcare provider will inquire about risk factors, such as smoking history, family history of lung disease, and any early signs of emphysema. A physical exam will check for signs of lung damage, including wheezing and abnormal lung sounds.
2. Alpha-1 Antitrypsin Deficiency Testing
Genetic testing to detect alpha-1 antitrypsin deficiency is key to confirming the diagnosis. This involves a blood test to measure A1PI levels and genetic screening to identify mutations in the SERPINA1 gene. Low levels of A1PI in the blood can confirm the presence of this deficiency.
3. Pulmonary Function Tests (PFTs)
Pulmonary function tests measure how well the lungs are working, assessing airflow, lung volume, and gas exchange. Reduced FEV1 (forced expiratory volume in one second) and FVC (forced vital capacity) values suggest the presence of emphysema.
4. Chest X-ray
A chest X-ray can reveal signs of emphysema, such as hyperinflated lungs, flattened diaphragms, and increased lung volume. However, a CT scan provides more detailed imaging and is more reliable in diagnosing emphysema.
5. CT Scan
A CT scan offers high-resolution images of the lungs and can show the extent of lung damage caused by emphysema. It can help differentiate between alpha-1-proteinase inhibitor deficiency-related emphysema and other forms of emphysema caused by smoking or environmental factors.
Treatment of Pulmonary Emphysema Associated with Alpha-1-Proteinase Inhibitor Deficiency
While there is no cure for emphysema associated with alpha-1-proteinase inhibitor deficiency, there are treatments available to manage symptoms, slow the progression of the disease, and improve quality of life.
1. Alpha-1-Proteinase Inhibitor Replacement Therapy
One of the most effective treatments for this condition is alpha-1-proteinase inhibitor replacement therapy. This involves regular infusions of purified A1PI, which helps neutralize neutrophil elastase and prevent further lung damage. This treatment is particularly beneficial in slowing the progression of emphysema.
2. Smoking Cessation
For individuals with emphysema who also smoke, quitting smoking is essential to prevent further lung damage. Smoking accelerates the progression of the disease and increases the risk of other complications, such as infections and COPD exacerbations.
3. Bronchodilators and Inhaled Corticosteroids
Medications such as bronchodilators help relax the muscles around the airways, improving airflow. Inhaled corticosteroids may also be prescribed to reduce inflammation in the airways and prevent flare-ups.
4. Oxygen Therapy
As emphysema worsens, oxygen therapy may be needed to ensure adequate oxygen levels in the bloodstream. This is especially necessary during physical activities or while sleeping, when oxygen levels may drop significantly.
5. Pulmonary Rehabilitation
Pulmonary rehabilitation is a structured program that includes physical exercises, education, and counseling. It helps patients with emphysema improve their physical fitness, manage symptoms, and improve their quality of life.
6. Lung Volume Reduction Surgery
In severe cases of emphysema, lung volume reduction surgery (LVRS) may be considered. LVRS involves removing damaged portions of the lung to improve the function of the remaining tissue. This surgery is generally recommended only for those who do not respond to other treatments.
7. Lung Transplantation
For individuals with advanced emphysema who are no longer responsive to other treatments, lung transplantation may be an option. This procedure involves replacing the damaged lungs with healthy ones from a donor.
Prevention of Pulmonary Emphysema
While emphysema related to alpha-1-proteinase inhibitor deficiency cannot always be prevented, there are several steps individuals can take to reduce the risk of developing severe symptoms:
1. Genetic Counseling and Early Diagnosis
For individuals with a family history of alpha-1-proteinase inhibitor deficiency, genetic counseling and early testing can help identify the condition before significant lung damage occurs. Early intervention is crucial in managing the disease and slowing its progression.
2. Avoid Smoking and Environmental Pollutants
For those at risk of emphysema, avoiding smoking and minimizing exposure to environmental pollutants, such as dust and chemicals, is critical to prevent further lung damage.
3. Vaccination
Vaccinations against respiratory infections, such as the flu and pneumonia, are vital for individuals with emphysema to prevent complications and exacerbations.
Pulmonary emphysema associated with alpha-1-proteinase inhibitor deficiency is a serious lung condition that requires early diagnosis and intervention. Genetic testing, along with appropriate treatment strategies like A1PI replacement therapy, smoking cessation, and pulmonary rehabilitation, can significantly improve the prognosis and quality of life for affected individuals. By managing the condition proactively, patients can slow disease progression and minimize the impact of pulmonary emphysema on their daily lives.