Pulmonary edema is a serious condition characterized by fluid accumulation in the lungs, leading to impaired oxygen exchange and difficulty breathing. When caused by chronic heart failure, pulmonary edema is a complex and progressive issue that significantly impacts the patient’s quality of life. Understanding the relationship between heart failure and pulmonary edema is essential for effective management and treatment. In this article, we explore the causes, symptoms, diagnosis, and treatment options for pulmonary edema due to chronic heart failure.
What is Pulmonary Edema?
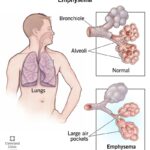
Pulmonary edema occurs when fluid builds up in the alveoli, the tiny air sacs in the lungs responsible for gas exchange. This fluid accumulation impairs the lungs’ ability to oxygenate the blood properly, leading to difficulty breathing, hypoxia, and respiratory distress. Pulmonary edema can result from a variety of conditions, but when it is due to chronic heart failure, the underlying issue is typically a compromised heart’s inability to effectively pump blood, causing fluid to back up in the lungs.
Chronic Heart Failure and Pulmonary Edema
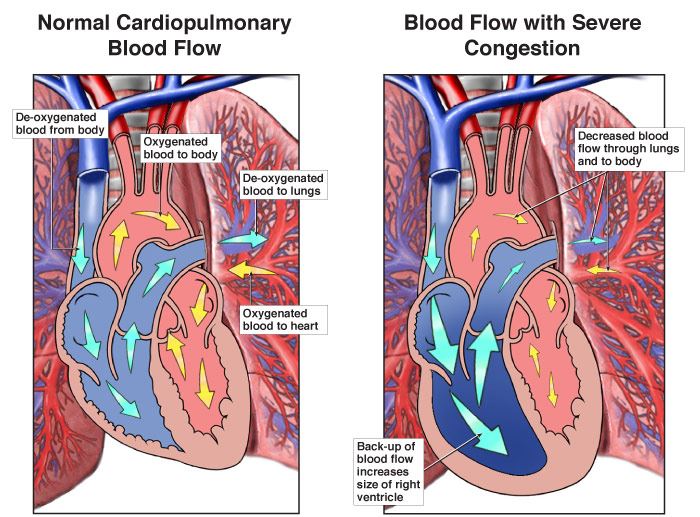
Chronic heart failure (CHF) is a long-term condition where the heart cannot pump blood effectively, leading to a reduction in blood flow to vital organs. This results in fluid buildup in the body, including the lungs, which can cause pulmonary edema. CHF is the most common cause of pulmonary edema, particularly in older adults.
There are two primary types of heart failure that can lead to pulmonary edema:
- Left-sided heart failure: When the left side of the heart cannot pump blood efficiently, blood backs up into the lungs, causing fluid buildup.
- Right-sided heart failure: Although right-sided heart failure primarily leads to fluid accumulation in the legs and abdomen, it can also contribute to pulmonary edema when it affects the left side of the heart.
Causes of Pulmonary Edema Due to Chronic Heart Failure
The development of pulmonary edema in individuals with chronic heart failure is primarily due to the heart’s inability to pump blood efficiently, which causes fluid to back up in the lungs. Several factors contribute to this process:
1. Impaired Left Ventricular Function
In left-sided heart failure, the left ventricle is weakened, resulting in a decreased ability to pump oxygenated blood into the systemic circulation. As the blood backs up into the pulmonary veins, pressure in the lungs increases, forcing fluid into the alveoli and causing pulmonary edema.
2. Increased Pulmonary Capillary Pressure
Chronic heart failure leads to increased pressure in the pulmonary capillaries, the small blood vessels that supply the lungs. When the heart fails to pump blood effectively, this increased pressure can push fluid into the lung tissues, causing swelling and fluid buildup.
3. Reduced Renal Function
Heart failure can reduce renal function, leading to fluid retention in the body. As the kidneys become less effective at removing excess fluid, this fluid can accumulate in the lungs, contributing to pulmonary edema.
4. Increased Sodium and Water Retention
The body’s response to heart failure includes activating mechanisms that promote sodium and water retention to increase blood volume. While this is initially compensatory, it eventually leads to excess fluid in the body, contributing to pulmonary edema.
5. Valvular Heart Disease
Conditions such as mitral valve stenosis or aortic valve regurgitation can impair the heart’s ability to pump blood effectively, leading to fluid backup in the lungs and increased risk of pulmonary edema.
Symptoms of Pulmonary Edema Due to Chronic Heart Failure
Pulmonary edema due to chronic heart failure presents with a range of symptoms that can worsen progressively. Common symptoms include:
1. Shortness of Breath
Shortness of breath (dyspnea) is one of the primary symptoms of pulmonary edema. It may be particularly noticeable during physical exertion or while lying flat (orthopnea). In severe cases, it can occur at rest.
2. Wheezing and Gasping for Air
Wheezing and a feeling of air hunger can occur as the airways become constricted due to fluid accumulation. These symptoms can worsen at night, leading to episodes of paroxysmal nocturnal dyspnea (PND).
3. Coughing and Frothy Sputum
Patients with pulmonary edema may experience coughing, often producing frothy sputum, which can be tinged with blood in more severe cases.
4. Fatigue and Weakness
Fluid buildup in the lungs can lead to decreased oxygen levels, causing fatigue and weakness, particularly during physical activities.
5. Rapid or Irregular Heartbeat
A rapid or irregular heartbeat (arrhythmia) can occur due to the strain on the heart caused by fluid buildup and poor circulation.
6. Swelling (Edema) in Other Areas
In addition to pulmonary edema, patients may experience swelling in the legs, ankles, or abdomen due to fluid retention, a common symptom of chronic heart failure.
Diagnosis of Pulmonary Edema Due to Chronic Heart Failure
Diagnosing pulmonary edema due to chronic heart failure involves a combination of physical examination, medical history review, and diagnostic tests. Healthcare providers will assess symptoms such as shortness of breath, cough, and fatigue, and may conduct the following tests:
1. Chest X-ray
A chest X-ray can reveal fluid buildup in the lungs, showing the classic “bat-wing” appearance of pulmonary edema. It can also help rule out other causes of shortness of breath, such as pneumonia.
2. Echocardiogram
An echocardiogram uses sound waves to create an image of the heart and evaluate its function. This test helps determine the severity of heart failure, measure ejection fraction, and identify issues such as valve problems or left ventricular dysfunction.
3. Electrocardiogram (ECG)
An ECG measures the electrical activity of the heart and can identify arrhythmias or other heart abnormalities that may contribute to heart failure and pulmonary edema.
4. Blood Tests
Blood tests can assess kidney function, electrolyte levels, and the presence of BNP (B-type natriuretic peptide), a hormone released in response to heart failure. Elevated BNP levels can help confirm the diagnosis of heart failure.
5. Pulmonary Artery Catheterization
In some cases, a pulmonary artery catheter may be used to directly measure pressures in the lungs and heart, providing valuable information about the extent of pulmonary edema and heart failure.
Treatment of Pulmonary Edema Due to Chronic Heart Failure
Treatment of pulmonary edema due to chronic heart failure focuses on managing both the fluid buildup and the underlying heart failure. Key treatment strategies include:
1. Oxygen Therapy
In mild to moderate cases of pulmonary edema, supplemental oxygen may be provided to help the patient breathe more easily and increase oxygen levels in the blood.
2. Diuretics
Diuretics are medications that help remove excess fluid from the body by increasing urine output. Furosemide (Lasix) is a commonly used diuretic for patients with pulmonary edema. It helps reduce fluid buildup in the lungs, alleviating symptoms.
3. Vasodilators
Vasodilators such as nitroglycerin can help reduce the pressure in the heart and lungs by relaxing blood vessels. This helps improve blood flow and decreases fluid accumulation.
4. Inotropes
In some cases, inotropic drugs like dobutamine may be used to increase the heart’s pumping ability. These drugs help improve cardiac output and reduce the severity of pulmonary edema.
5. ACE Inhibitors and ARBs
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are commonly prescribed to treat chronic heart failure. These medications help relax blood vessels, reduce fluid retention, and decrease the heart’s workload.
6. Lifestyle Modifications
Patients with chronic heart failure are advised to make lifestyle changes such as reducing salt intake, maintaining a healthy weight, quitting smoking, and exercising regularly to manage their condition effectively.
Prevention of Pulmonary Edema Due to Chronic Heart Failure
Preventing pulmonary edema involves managing heart failure and reducing the risk of complications. Key strategies include:
1. Proper Management of Heart Failure
Effective management of chronic heart failure through medication, regular monitoring, and lifestyle modifications is essential for preventing the onset of pulmonary edema.
2. Monitoring Fluid Intake
Carefully monitoring fluid intake and output is important for patients with chronic heart failure. Limiting fluid intake and taking prescribed diuretics as directed can help prevent fluid overload.
3. Regular Check-ups
Regular visits to a healthcare provider can help monitor the progression of heart failure and identify early signs of pulmonary edema, allowing for prompt intervention.
4. Vaccination
Vaccinations against influenza and pneumonia can reduce the risk of respiratory infections, which can exacerbate pulmonary edema and heart failure.
Pulmonary edema due to chronic heart failure is a serious condition that requires prompt diagnosis and treatment to prevent complications and improve quality of life. By understanding the causes, symptoms, diagnosis, and treatment options, individuals and healthcare providers can work together to manage this condition effectively. Early intervention, combined with lifestyle changes and appropriate medications, can help reduce the burden of pulmonary edema and improve outcomes for patients with chronic heart failure.