Pulmonary coccidioidomycosis, commonly known as Valley fever, is a fungal infection caused by the Coccidioides species. This disease primarily affects the lungs but can spread to other parts of the body, resulting in a condition known as disseminated coccidioidomycosis. While coccidioidomycosis is generally endemic to arid regions of the southwestern United States, parts of Mexico, and Central and South America, it can affect anyone exposed to the Coccidioides fungi. Understanding its causes, symptoms, diagnosis, treatment, and prevention strategies is essential for managing this potentially serious infection.
What is Pulmonary Coccidioidomycosis?
Pulmonary coccidioidomycosis is a fungal infection that primarily affects the lungs. The infection is caused by inhaling Coccidioides spores, which are found in soil in areas where the fungi are endemic. These spores can become airborne during disturbances such as dust storms, construction activities, or even outdoor recreational activities. Once inhaled, the spores can lead to an infection that primarily affects the lungs, but it may spread to other organs in the body, particularly in individuals with weakened immune systems.
Causes and Risk Factors
Pulmonary coccidioidomycosis is caused by the Coccidioides species, which are dimorphic fungi found in arid climates. The two most common species responsible for this infection are Coccidioides immitis and Coccidioides posadasii. These fungi are typically found in soil in specific regions, including parts of Arizona, California, Nevada, New Mexico, Texas, and northern Mexico.
1. Transmission via Inhalation
The primary mode of transmission is the inhalation of airborne Coccidioides spores. These spores are released into the air when soil is disturbed, such as during construction, farming, or dust storms. Once inhaled, the spores can settle in the lungs, where they begin to grow and reproduce.
2. Environmental Factors
Areas with dry, dusty conditions are the most conducive to the growth and spread of Coccidioides spores. Warm, arid regions such as the southwestern United States, parts of Mexico, and some areas of Central and South America are considered endemic to the fungus. The fungi thrive in desert soils, and outbreaks often occur after heavy rainfall followed by dry conditions, which promote the growth of the spores.
3. Risk Factors for Infection
While anyone living or working in endemic areas can be at risk, certain individuals are more susceptible to severe infection:
- Individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or those on immunosuppressive therapy.
- Pregnant women are at a higher risk, particularly in the second or third trimester.
- People of certain racial or ethnic backgrounds, such as African Americans, Filipinos, and Native Americans, are more likely to experience severe forms of the disease.
Symptoms of Pulmonary Coccidioidomycosis
The symptoms of pulmonary coccidioidomycosis can range from mild to severe, and some individuals may remain asymptomatic. When symptoms occur, they may resemble those of other respiratory conditions, such as pneumonia or bronchitis. Common symptoms include:
1. Cough
A persistent cough is one of the most common symptoms of pulmonary coccidioidomycosis. The cough may produce mucus or be dry in nature and may be associated with chest pain.
2. Fever
Fever is frequently observed, often accompanied by chills. This is a typical response of the body to the fungal infection as the immune system attempts to fight off the invading pathogen.
3. Fatigue and Malaise
Many individuals with pulmonary coccidioidomycosis report feeling fatigued and unwell, even when other symptoms are not severe. This can be due to the body’s inflammatory response to the infection.
4. Shortness of Breath
As the infection progresses, individuals may experience difficulty breathing or shortness of breath, particularly during physical activity.
5. Chest Pain
Pain or discomfort in the chest, often exacerbated by deep breathing or coughing, is another symptom of pulmonary coccidioidomycosis. This is typically due to inflammation in the lung tissue.
6. Night Sweats
Night sweats are common in individuals with more severe or disseminated forms of the disease.
7. Rash
Some individuals, especially those with disseminated coccidioidomycosis, may develop a rash, which can be a sign that the infection has spread beyond the lungs.
Diagnosis of Pulmonary Coccidioidomycosis
Diagnosing pulmonary coccidioidomycosis typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. The process begins with an assessment of symptoms and a review of the patient’s medical history, especially if they have recently traveled to or live in an endemic area.
1. Laboratory Tests
- Serology: Blood tests that detect antibodies against Coccidioides can help confirm the diagnosis. These tests can detect IgM and IgG antibodies, which are typically present during an active infection.
- Culture: The Coccidioides fungus can be cultured from sputum, lung tissue, or other bodily fluids, although this is not always practical due to the time it takes for fungal cultures to grow.
- PCR (Polymerase Chain Reaction): PCR testing can be used to detect the genetic material of Coccidioides, which helps to confirm the diagnosis, especially in cases with negative serology.
2. Imaging Studies
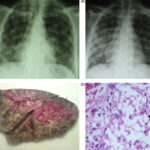
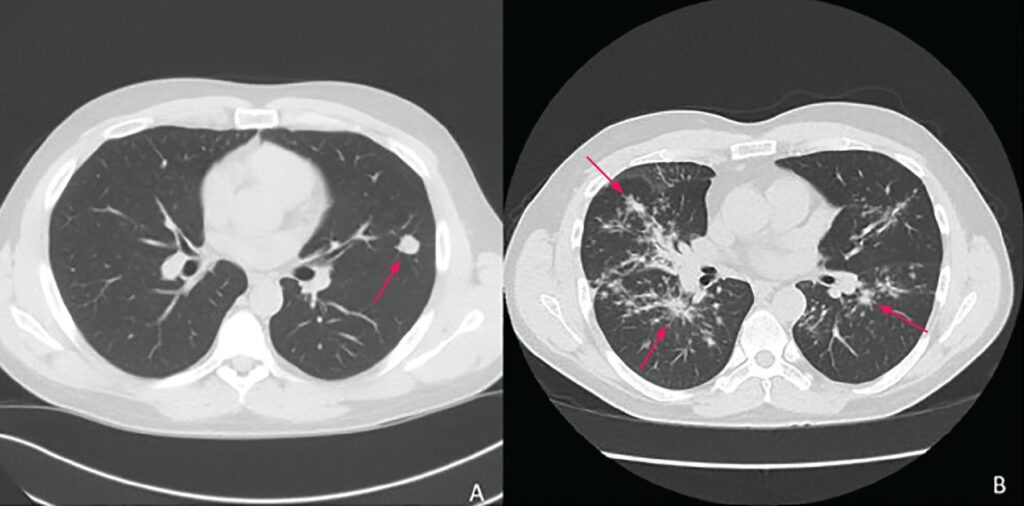
- Chest X-ray: A chest X-ray may reveal abnormal patterns in the lungs, such as consolidation or nodules, which are common signs of pulmonary coccidioidomycosis.
- CT Scan: A high-resolution CT scan of the chest may provide more detailed information about lung involvement, revealing nodules, cavities, or lymphadenopathy.
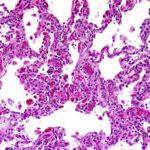
3. Biopsy
In rare cases where the diagnosis is uncertain, a biopsy of lung tissue may be necessary to confirm the presence of Coccidioides organisms.
Treatment of Pulmonary Coccidioidomycosis
Most cases of pulmonary coccidioidomycosis are mild and resolve without the need for treatment. However, in more severe cases, antifungal medications are required.
1. Antifungal Therapy
- Fluconazole and itraconazole are commonly used antifungal medications for treating pulmonary coccidioidomycosis. These medications are typically prescribed for several months to prevent relapse and manage symptoms.
- Amphotericin B may be used for severe cases, particularly when there is dissemination of the infection to other organs, or when the patient is immunocompromised.
2. Supportive Care
For mild cases, supportive care such as rest, fluids, and over-the-counter pain relievers to alleviate fever and chest discomfort may be sufficient. Patients with more severe disease may require hospitalization and oxygen therapy to assist with breathing.
3. Surgical Intervention
In cases where there is significant lung damage or an abscess, surgical intervention may be necessary to remove the affected tissue. This is a rare option and is typically considered only after other treatments have failed.
Prevention of Pulmonary Coccidioidomycosis
Preventing pulmonary coccidioidomycosis is challenging, as it primarily relies on avoiding exposure to the airborne spores of Coccidioides. However, several strategies can help reduce the risk of infection, especially for those living or working in endemic areas.
1. Limit Exposure to Dust
Individuals in endemic regions should avoid outdoor activities during dust storms or when soil is being disturbed, such as during construction or agricultural work. Wearing masks may offer some protection in high-risk environments.
2. Personal Protective Equipment (PPE)
For those working in environments with a high risk of fungal exposure, such as construction sites or archaeological digs, wearing protective masks and other PPE can reduce the likelihood of inhaling the spores.
3. Public Health Measures
Public health initiatives to reduce soil disturbance and promote awareness of coccidioidomycosis are critical in endemic areas to minimize the spread of the infection.
Pulmonary coccidioidomycosis is a serious fungal infection with a wide range of symptoms and potential complications. Though it is most common in arid regions, it can affect anyone exposed to the Coccidioides fungi. Early detection through appropriate diagnostic methods, combined with effective antifungal treatments, can significantly improve outcomes for patients. Preventive measures, including limiting exposure to dust and using protective equipment, are essential for those living or working in endemic areas. Understanding this infection and its management is key to reducing its impact on public health.