Pulmonary capillary hemangiomatosis (PCH) is an extremely rare lung disorder characterized by the abnormal growth of blood vessels in the pulmonary capillaries. This condition results in the formation of capillary-like blood vessels within the lungs, leading to significant changes in lung structure and function. While the disease is not widely known, its potential for causing severe respiratory issues necessitates an in-depth understanding of its pathophysiology, clinical presentation, diagnosis, and treatment options.
What is Pulmonary Capillary Hemangiomatosis?
Pulmonary capillary hemangiomatosis is a condition where there is an abnormal proliferation of small blood vessels in the lungs. These capillaries become enlarged and can cause vascular malformations. This malformation leads to impaired oxygen exchange within the lungs, contributing to the various clinical symptoms observed in affected individuals. Though rare, this disease can be quite severe, and early detection is crucial for managing its progression.
Causes of Pulmonary Capillary Hemangiomatosis
The exact cause of pulmonary capillary hemangiomatosis remains unclear, but the disease is thought to arise from an abnormality in the vascular endothelial cells of the lungs. Some of the known factors that may contribute to its development include:
1. Genetic Factors
In some cases, genetic mutations may play a role in the development of pulmonary capillary hemangiomatosis. The condition has been associated with certain genetic syndromes, such as familial pulmonary arterial hypertension (PAH). It is hypothesized that mutations in genes that regulate angiogenesis, the process of new blood vessel formation, may contribute to the formation of abnormal blood vessels in the lungs.
2. Environmental Factors
Though genetic factors are significant, environmental influences such as chronic exposure to pollutants, toxins, or infections may also trigger the development of vascular malformations in the lungs. However, the role of environmental factors in PCH remains speculative.
3. Underlying Diseases
Pulmonary capillary hemangiomatosis can sometimes be seen in association with other diseases, particularly pulmonary arterial hypertension (PAH). It is also observed in some patients with conditions like systemic sclerosis or other connective tissue diseases, which could predispose individuals to vascular abnormalities.
Symptoms of Pulmonary Capillary Hemangiomatosis
The clinical presentation of pulmonary capillary hemangiomatosis can vary depending on the extent of vascular involvement and the individual’s overall health. The most common symptoms include:
1. Shortness of Breath
Due to the compromised lung function caused by abnormal blood vessels, individuals with PCH often experience dyspnea (shortness of breath). This can range from mild breathlessness during physical activity to severe shortness of breath at rest in advanced stages.
2. Chronic Cough
Patients with PCH may develop a persistent dry cough. This symptom is typically caused by the changes in lung structure and the resulting inflammation in the pulmonary capillaries.
3. Fatigue and Weakness
As the lung’s ability to oxygenate blood becomes impaired, individuals with PCH may experience chronic fatigue and weakness. This is often due to decreased oxygen delivery to tissues and organs throughout the body.
4. Hemoptysis
In severe cases, pulmonary capillary hemangiomatosis can lead to hemoptysis, or coughing up blood. This may occur due to ruptures in the abnormal blood vessels within the lungs, leading to bleeding into the airways.
5. Cyanosis
As a result of inadequate oxygenation, some individuals may experience cyanosis, a bluish discoloration of the skin, particularly in the lips, fingers, and toes. This is an indication of insufficient oxygen levels in the blood.
Diagnosis of Pulmonary Capillary Hemangiomatosis
The diagnosis of pulmonary capillary hemangiomatosis involves a combination of clinical evaluation, imaging studies, and histopathological analysis.
1. Medical History and Physical Examination
The diagnostic process begins with a thorough medical history and physical examination. Doctors will inquire about the patient’s symptoms, such as shortness of breath, cough, and fatigue, and assess for signs of respiratory distress.
2. Imaging Studies
Imaging plays a crucial role in identifying the structural changes in the lungs associated with PCH. Key imaging techniques include:
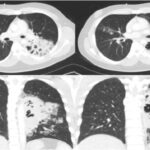
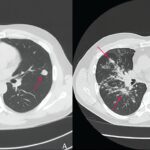
- Chest X-ray: Though not always definitive, a chest X-ray may show nonspecific findings, such as increased vascular markings in the lungs.
- High-Resolution CT (HRCT) Scan: HRCT scans provide more detailed images of the lungs and may reveal characteristic signs of pulmonary capillary hemangiomatosis, such as diffuse nodular opacities, vascular enlargement, and signs of pulmonary hypertension.
- Magnetic Resonance Imaging (MRI): MRI may be used to provide additional information on lung structures and blood vessels, especially in cases where vascular malformations are suspected.
3. Pulmonary Function Tests (PFTs)
Pulmonary function tests are important for assessing lung capacity and functionality. These tests measure parameters like lung volumes, gas exchange efficiency, and airflow. Reduced lung function is often seen in individuals with PCH.
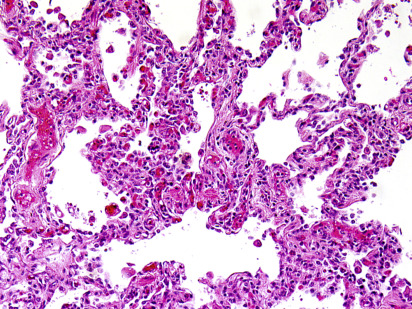
4. Biopsy and Histopathology
A definitive diagnosis of pulmonary capillary hemangiomatosis is usually confirmed through a lung biopsy. Histopathological examination of the tissue samples reveals characteristic capillary-like vessels and signs of vascular proliferation. Immunohistochemical staining can also be used to identify specific markers for blood vessel endothelial cells.
Treatment of Pulmonary Capillary Hemangiomatosis
There is no one-size-fits-all treatment for pulmonary capillary hemangiomatosis, as management depends on the severity of the disease, the patient’s overall health, and the presence of any comorbid conditions. However, several treatment options are available.
1. Oxygen Therapy
In cases of severe hypoxemia (low blood oxygen levels), supplemental oxygen therapy is often required to maintain oxygen saturation in the blood. This is particularly important for individuals experiencing shortness of breath and cyanosis.
2. Pulmonary Vasodilators
Pulmonary vasodilators, such as prostacyclin analogs and endothelin receptor antagonists, may be used to manage pulmonary hypertension associated with PCH. These medications help relax the blood vessels in the lungs, improving blood flow and oxygen exchange.
3. Corticosteroids
In some cases, corticosteroids may be prescribed to reduce inflammation in the lungs, especially when there is evidence of inflammation or autoimmune involvement. Steroids help control the inflammatory response that may be contributing to the vascular malformations.
4. Lung Transplantation
In advanced or refractory cases of pulmonary capillary hemangiomatosis, where other treatments have failed to provide relief, lung transplantation may be considered. This option is reserved for individuals with severe lung damage and progressive respiratory failure.
5. Antifungal or Antiviral Treatment (If Applicable)
If an underlying infection is suspected, antifungal or antiviral medications may be prescribed. These are particularly important if there is evidence of a secondary infection exacerbating the lung condition.
Prognosis of Pulmonary Capillary Hemangiomatosis
The prognosis for individuals with pulmonary capillary hemangiomatosis depends largely on the severity of the disease at the time of diagnosis and the effectiveness of treatment. Early detection and management can improve quality of life and help prevent complications such as pulmonary hypertension and respiratory failure. In more advanced stages, when the disease has caused significant damage to the lungs, the prognosis may be less favorable, and patients may require ongoing respiratory support or even lung transplantation.
Prevention of Pulmonary Capillary Hemangiomatosis
As a rare disease with unclear causation, there are no specific preventive measures for pulmonary capillary hemangiomatosis. However, reducing exposure to known risk factors, such as environmental toxins and managing underlying conditions like pulmonary arterial hypertension, may help lower the risk of developing vascular lung diseases.
Pulmonary capillary hemangiomatosis is a rare but serious vascular disorder that affects the lungs. Due to its potential for severe respiratory compromise, early detection and appropriate treatment are crucial for improving outcomes. While the exact cause remains uncertain, advancements in diagnostic techniques and treatment options offer hope for managing the disease and enhancing patient quality of life. Understanding the symptoms, diagnostic process, and treatment strategies is essential for healthcare professionals and patients alike in managing this complex condition.