Pulmonary aspergillosis refers to a spectrum of lung infections caused by the fungus Aspergillus. This condition primarily affects individuals with weakened immune systems, chronic lung diseases, or pre-existing respiratory conditions. The infection can range from mild, asymptomatic cases to severe and life-threatening situations, especially in immunocompromised individuals. Early detection, proper diagnosis, and effective treatment are crucial in managing pulmonary aspergillosis and preventing complications.
What is Pulmonary Aspergillosis?
Pulmonary aspergillosis is a fungal infection caused by the Aspergillus species, a mold commonly found in the environment, particularly in decaying organic matter, soil, and plant debris. The most common type of Aspergillus that causes pulmonary infections is Aspergillus fumigatus. In healthy individuals, Aspergillus spores are usually harmless as the immune system can effectively prevent infection. However, in individuals with weakened immunity or pre-existing lung conditions, the fungus can cause severe infections in the lungs.
Causes and Risk Factors of Pulmonary Aspergillosis
1. Immunocompromised States
The most significant risk factor for pulmonary aspergillosis is immunosuppression, which weakens the body’s natural defense mechanisms. Common conditions that predispose individuals to this infection include:
- HIV/AIDS: A weakened immune system due to HIV can increase susceptibility to fungal infections like aspergillosis.
- Chemotherapy or Organ Transplants: Immunosuppressive medications used to treat cancer or prevent organ rejection after a transplant can suppress the immune system, making patients more vulnerable to infections.
- Corticosteroid Use: Prolonged use of steroids to manage chronic conditions such as asthma, rheumatoid arthritis, or lupus can impair immune function.
2. Chronic Respiratory Diseases
Individuals with chronic lung diseases are at higher risk of developing pulmonary aspergillosis due to the existing damage to the lung tissue. Conditions such as:
- Chronic Obstructive Pulmonary Disease (COPD)
- Cystic Fibrosis
- Tuberculosis (TB) These diseases often create a favorable environment for Aspergillus to infect the lungs and worsen respiratory function.
3. Environmental Exposure
Exposure to large quantities of Aspergillus spores, especially in certain occupational settings, can increase the risk of infection. These environments include:
- Farmers or agricultural workers exposed to soil or hay that contains the fungus.
- Construction workers exposed to moldy building materials.
- Moldy indoor environments can also contribute to chronic exposure, particularly for individuals living in damp or poorly ventilated areas.
Symptoms of Pulmonary Aspergillosis
The symptoms of pulmonary aspergillosis can vary significantly depending on the individual’s overall health, immune system status, and the severity of the infection. Common symptoms include:
1. Chronic Cough and Wheezing
A persistent cough, often accompanied by wheezing, is one of the hallmark symptoms of pulmonary aspergillosis. This occurs as the infection irritates the airways and triggers an inflammatory response.
2. Shortness of Breath (Dyspnea)
As the infection progresses, patients may experience difficulty breathing, particularly during physical activity. This is due to inflammation and damage to the lung tissue caused by the fungal infection.
3. Chest Pain
Individuals with pulmonary aspergillosis may experience localized chest pain or discomfort, especially during deep breathing or coughing. This pain is often due to inflammation of the lung lining or pleura.
4. Fatigue and Malaise
Chronic fatigue, generalized weakness, and a feeling of being unwell (malaise) are common symptoms. These symptoms result from the body’s ongoing battle against the infection, leading to overall system-wide exhaustion.
5. Hemoptysis (Coughing up Blood)
In more severe cases, pulmonary aspergillosis may lead to hemoptysis, or coughing up blood, which is a sign of significant lung damage or the formation of fungal balls in the airways.
6. Fever
While not always present, fever can occur, particularly if the infection becomes more widespread or causes significant inflammation in the lungs.
Types of Pulmonary Aspergillosis
Pulmonary aspergillosis can manifest in several distinct forms, each with unique characteristics and treatment strategies.
1. Allergic Bronchopulmonary Aspergillosis (ABPA)
ABPA is an allergic reaction to Aspergillus that primarily affects individuals with asthma or cystic fibrosis. In this form, the immune system overreacts to the presence of Aspergillus, leading to inflammation and damage in the airways. Symptoms include wheezing, coughing, and shortness of breath.
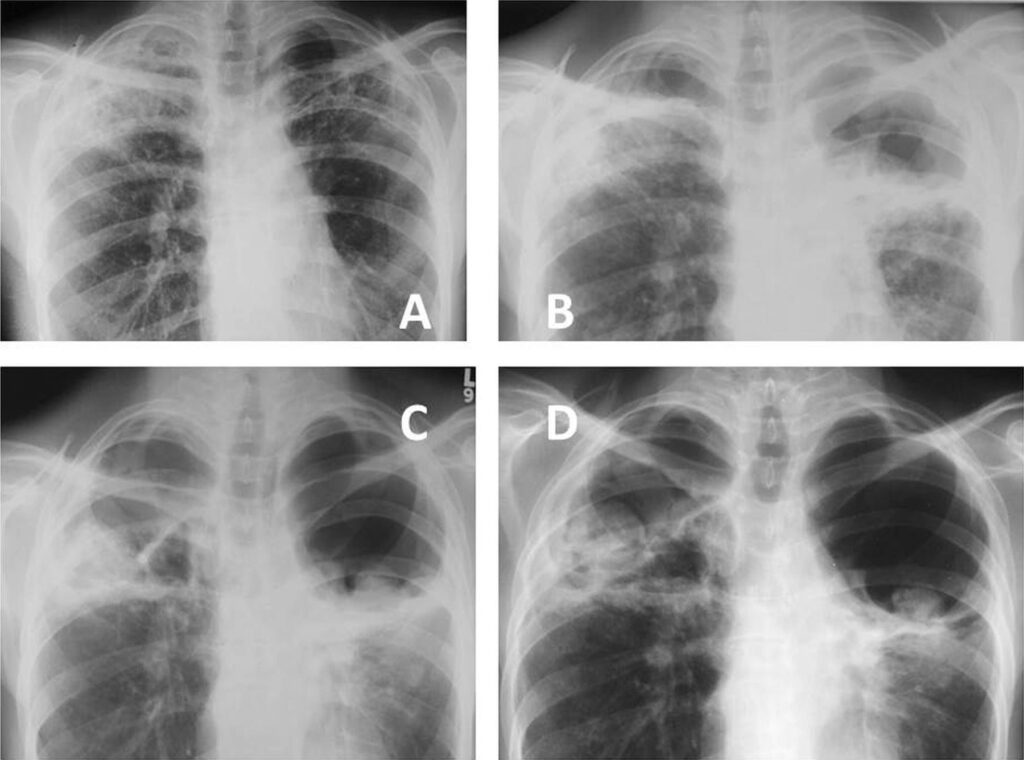
2. Chronic Pulmonary Aspergillosis (CPA)
CPA typically occurs in individuals with pre-existing lung diseases such as tuberculosis or COPD. It leads to the formation of fungal balls (aspergillomas) in the lungs. Symptoms of CPA are often mild and may include a chronic cough, fatigue, and coughing up blood.
3. Invasive Pulmonary Aspergillosis (IPA)
IPA is a severe and life-threatening form of the disease that occurs in immunocompromised individuals. The fungus invades the lung tissue and spreads rapidly, leading to tissue destruction and the formation of abscesses. Symptoms include high fever, shortness of breath, and severe chest pain. IPA requires immediate medical intervention and antifungal therapy.
Diagnosing Pulmonary Aspergillosis
Accurate diagnosis of pulmonary aspergillosis involves a combination of clinical evaluation, imaging studies, and laboratory tests.
1. Medical History and Physical Examination
A detailed medical history is essential for identifying risk factors and determining whether the patient has any pre-existing conditions that might predispose them to fungal infections. During the physical examination, doctors assess for signs of respiratory distress, chest pain, or abnormal breath sounds.
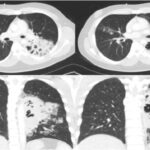
2. Imaging Studies
Chest X-rays and computed tomography (CT) scans are essential tools for diagnosing pulmonary aspergillosis. In cases of CPA, imaging may reveal the presence of aspergillomas (fungal balls), while in IPA, more extensive lung damage, consolidation, and cavitary lesions may be observed.
3. Microbiological Cultures
Sputum or bronchoalveolar lavage (BAL) samples are collected to identify the presence of Aspergillus species. Fungal cultures and PCR testing can confirm the diagnosis by detecting fungal DNA in the respiratory tract.
4. Serologic Tests
Blood tests can help detect antibodies or antigens associated with Aspergillus, supporting the diagnosis of ABPA. However, these tests are less useful for diagnosing CPA or IPA.
5. Histopathological Examination
In more severe cases, tissue biopsies may be performed to directly examine lung tissue for signs of fungal invasion, particularly in invasive pulmonary aspergillosis.
Treatment Options for Pulmonary Aspergillosis
The treatment of pulmonary aspergillosis depends on the type of infection and the patient’s overall health. Options include antifungal medications, corticosteroids, and sometimes surgical intervention.
1. Antifungal Medications
The cornerstone of treatment for pulmonary aspergillosis is antifungal therapy. Common antifungal drugs include:
- Voriconazole: Considered the treatment of choice for invasive pulmonary aspergillosis, this medication is effective in combating the infection and preventing further lung damage.
- Itraconazole and Posaconazole: These medications are often used for chronic pulmonary aspergillosis or in cases where voriconazole is not effective.
- Amphotericin B: This intravenous drug is used in severe cases of IPA, particularly when other treatments fail.
2. Corticosteroids
In cases of allergic bronchopulmonary aspergillosis (ABPA), corticosteroids are used to manage inflammation and control allergic reactions. These medications help reduce airway inflammation and improve symptoms like wheezing and coughing.
3. Surgical Intervention
In cases where aspergillomas (fungal balls) are present, or in cases of severe tissue damage from invasive aspergillosis, surgical removal of the fungal mass or affected lung tissue may be necessary.
4. Supportive Care
Supportive care is important for improving patient outcomes, particularly in severe cases. This may include oxygen therapy to support breathing, pulmonary rehabilitation, and nutritional support to enhance recovery.
Prognosis and Prevention
The prognosis of pulmonary aspergillosis varies widely depending on the type of infection, the patient’s underlying health, and the timeliness of treatment. While allergic bronchopulmonary aspergillosis can often be managed effectively with medication, chronic pulmonary aspergillosis and invasive pulmonary aspergillosis can be life-threatening if not treated promptly.
Prevention involves minimizing exposure to Aspergillus spores, especially in high-risk individuals. This may include avoiding dusty environments, wearing protective masks in occupational settings, and managing underlying conditions to reduce immune suppression.
Pulmonary aspergillosis is a serious condition that requires early diagnosis and effective treatment to prevent severe complications. By understanding its causes, symptoms, and treatment options, healthcare providers can help improve patient outcomes and quality of life. Advances in antifungal therapy and other medical interventions continue to offer hope for patients suffering from this challenging disease.