Pulmonary actinomycosis is a rare but serious bacterial infection that affects the lungs, primarily caused by Actinomyces species. It is a type of actinomycosis, a condition that typically manifests in the cervicofacial region, but can also affect the chest, abdomen, and pelvis. This lung infection often presents with symptoms resembling more common respiratory illnesses, making it challenging to diagnose promptly. Understanding the pathophysiology, symptoms, diagnosis, and treatment options for pulmonary actinomycosis is essential for proper management and improved patient outcomes.
Causes of Pulmonary Actinomycosis
Pulmonary actinomycosis is caused by Actinomyces, a genus of gram-positive, anaerobic bacteria that are normally found in the mouth, throat, and gastrointestinal tract. While these bacteria are typically harmless when confined to their normal habitats, they can become pathogenic when they enter deeper tissues due to trauma, surgical procedures, or other factors that compromise the body’s natural barriers.
The most common causes and risk factors for pulmonary actinomycosis include:
- Aspiration pneumonia: Inhalation of oral or gastrointestinal contents can introduce Actinomyces bacteria into the lungs, leading to infection.
- Chronic lung diseases: Conditions like tuberculosis or COPD (chronic obstructive pulmonary disease) can create a favorable environment for the growth of Actinomyces bacteria.
- Immunosuppression: People with weakened immune systems, such as those with HIV/AIDS or those undergoing chemotherapy, are more susceptible to actinomycosis.
- Dental infections: Poor oral hygiene and untreated dental issues can lead to the spread of Actinomyces from the mouth to the lungs.
- Trauma or surgery: Invasive procedures involving the chest or throat can introduce Actinomyces bacteria into the lung tissue, increasing the risk of infection.
Symptoms of Pulmonary Actinomycosis
The symptoms of pulmonary actinomycosis can be vague and may resemble those of other more common lung infections. They often develop slowly over weeks or months, making early diagnosis difficult. Common symptoms include:
- Chronic cough: A persistent cough is one of the hallmark symptoms of pulmonary actinomycosis. It may initially be dry but can eventually produce purulent sputum.
- Chest pain: Pain in the chest, often sharp and localized, may occur due to inflammation in the lung tissue.
- Fever and night sweats: These systemic symptoms are common in infections and may indicate an ongoing inflammatory response.
- Shortness of breath (dyspnea): Difficulty breathing can arise as the infection progresses and affects lung function.
- Weight loss and fatigue: Chronic infections like pulmonary actinomycosis can lead to general malaise, weight loss, and a feeling of extreme tiredness.
- Hemoptysis (coughing up blood): In more severe cases, bleeding in the lungs can occur, resulting in blood-tinged sputum.
These symptoms may be mistaken for other respiratory conditions, including tuberculosis, pneumonia, or lung cancer, which is why a thorough evaluation is crucial for accurate diagnosis.
Diagnosis of Pulmonary Actinomycosis
Diagnosing pulmonary actinomycosis requires a combination of clinical suspicion, imaging studies, and microbiological tests. Due to the nonspecific nature of the symptoms, it is often misdiagnosed as other more common respiratory diseases. The diagnostic process typically includes:
1. Clinical Evaluation
A detailed history and physical examination are essential. The healthcare provider will assess symptoms such as the duration of the cough, the presence of chest pain, and the occurrence of systemic symptoms like fever or weight loss. The patient’s medical history, including risk factors such as dental problems or previous respiratory infections, will also be taken into account.
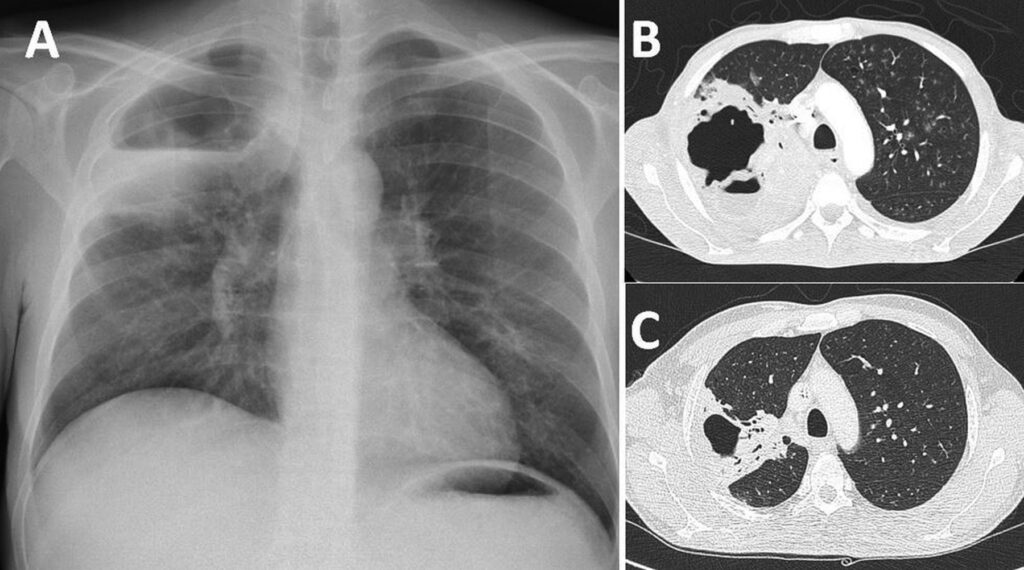
2. Chest X-ray or CT Scan
Imaging studies are crucial in visualizing the extent of lung involvement. A chest X-ray may reveal consolidation, cavitary lesions, or pleural effusion, which are suggestive of pulmonary actinomycosis. A more detailed CT scan of the chest can provide better insight into the location and size of the infection, as well as the presence of any abscesses or masses.
3. Microbiological Testing
The gold standard for diagnosing pulmonary actinomycosis is the identification of Actinomyces bacteria through culture. Sputum samples, bronchoalveolar lavage fluid, or biopsies from lung tissue may be collected and cultured in a laboratory to confirm the presence of the bacteria. However, Actinomyces can be slow-growing, and cultures may take several weeks to yield results. Additionally, PCR (polymerase chain reaction) tests may be used for rapid detection of bacterial DNA.
4. Histopathological Examination
In cases of suspected pulmonary actinomycosis, tissue biopsy may be performed to obtain a definitive diagnosis. The characteristic presence of sulfur granules, which are clumps of bacterial colonies, can be observed under the microscope, aiding in diagnosis.
Treatment of Pulmonary Actinomycosis
The treatment of pulmonary actinomycosis primarily involves the use of antibiotics. The choice of antibiotics and the duration of treatment depend on the severity of the infection and the overall health of the patient. Commonly used antibiotics include:
1. Penicillin
Penicillin is the first-line treatment for pulmonary actinomycosis due to its effectiveness against Actinomyces species. Treatment often begins with intravenous penicillin, followed by oral penicillin or amoxicillin once the patient shows signs of improvement.
2. Alternative Antibiotics
For patients who are allergic to penicillin or who have penicillin-resistant strains, alternative antibiotics may be prescribed, such as tetracyclines (e.g., doxycycline), clindamycin, or macrolides (e.g., erythromycin).
3. Surgical Intervention
In cases where there is extensive lung tissue damage, abscess formation, or the presence of a large mass, surgery may be necessary to remove infected tissue or drain abscesses. Surgery is generally considered if antibiotic therapy alone is insufficient to control the infection.
4. Supportive Care
In addition to antibiotics, supportive care is essential in managing symptoms and promoting recovery. This may include pain management, oxygen therapy for patients with severe shortness of breath, and nutritional support for those experiencing weight loss and fatigue.
Prognosis and Outlook
With early diagnosis and appropriate antibiotic treatment, the prognosis for pulmonary actinomycosis is generally favorable. Most patients recover completely, although the infection can be challenging to treat in immunocompromised individuals or those with extensive lung involvement. If left untreated, pulmonary actinomycosis can lead to severe complications, including lung abscesses, fibrosis, or even respiratory failure.
Prevention of Pulmonary Actinomycosis
Preventing pulmonary actinomycosis primarily involves reducing risk factors associated with the infection. Some preventive measures include:
- Good oral hygiene: Regular dental checkups and maintaining good oral health can help prevent the spread of Actinomyces bacteria from the mouth to the lungs.
- Avoiding aspiration: Taking precautions to prevent aspiration, particularly in patients with swallowing difficulties, can reduce the risk of introducing bacteria into the lungs.
- Prompt treatment of respiratory infections: Early and aggressive treatment of conditions like pneumonia or tuberculosis can help prevent secondary infections like actinomycosis.
Pulmonary actinomycosis, though rare, is a serious lung infection that requires prompt diagnosis and treatment to prevent complications. Understanding the causes, symptoms, and treatment options for this condition is essential for effective management. By recognizing the signs of pulmonary actinomycosis early and employing appropriate antibiotic therapy, most patients can achieve a full recovery and return to normal activities.