Pseudomonas aeruginosa, a gram-negative opportunistic pathogen, is a leading cause of osteomyelitis, especially in immunocompromised patients or following trauma and surgical procedures. Known for its biofilm-forming capacity and antibiotic resistance, this bacterium complicates bone infections and presents significant therapeutic challenges.
Pathogenesis and Infection Mechanisms
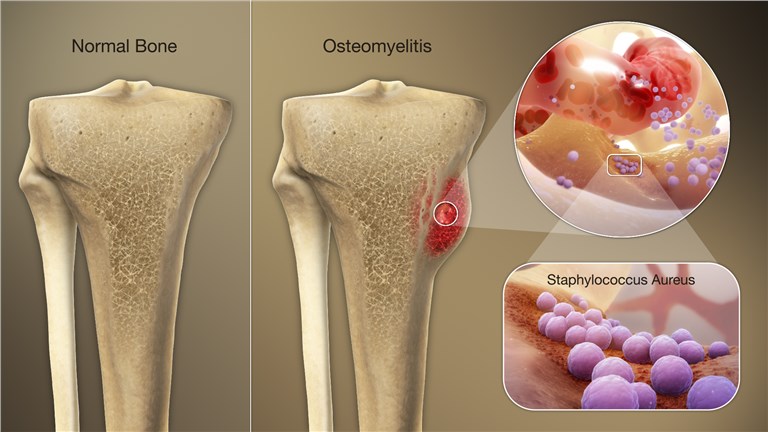
Pseudomonas aeruginosa initiates osteomyelitis through hematogenous spread, contiguous infection from nearby tissues, or direct inoculation during surgery or trauma. Once established, it adheres to bone surfaces and forms biofilms—structured bacterial communities encapsulated in extracellular polymeric substances (EPS)—that protect it from host immune defenses and antimicrobial agents.
Risk Factors and Vulnerable Populations
- Diabetic foot infections
- Open fractures and orthopedic implants
- Intravenous drug use
- Immunosuppression (e.g., chemotherapy, HIV)
- Peripheral vascular disease
- Previous surgical interventions
Clinical Presentation
Patients with P. aeruginosa osteomyelitis may present acutely or chronically, depending on the infection’s origin and progression.
Common symptoms include:
- Persistent localized pain
- Swelling, redness, or warmth over affected area
- Fever and malaise (more in acute cases)
- Sinus tract formation (in chronic cases)
- Purulent discharge
Diagnostic Evaluation
Timely diagnosis is critical to prevent irreversible bone damage. The diagnostic process should be systematic and multifactorial.
Imaging Studies
- X-ray: Initial screening but limited in early stages
- MRI: Gold standard for early detection, shows marrow edema and abscesses
- CT scan: Useful for cortical bone evaluation
- Nuclear medicine: Technetium-99m bone scan and labeled leukocyte scans in complex cases
Laboratory Markers
- Elevated ESR and CRP
- Leukocytosis in acute phases
- Blood cultures may reveal bacteremia
Microbiological Confirmation
- Bone biopsy and culture: Definitive diagnosis and guide for antimicrobial therapy
- Wound swabs: Less reliable due to surface contamination
Antimicrobial Resistance Challenges
Pseudomonas aeruginosa demonstrates intrinsic and acquired resistance to multiple antibiotic classes, including beta-lactams, aminoglycosides, and fluoroquinolones. Resistance mechanisms include:
- Efflux pumps
- Beta-lactamase production
- Porin loss
- Biofilm-mediated resistance
Treatment Strategies
Empirical and Targeted Antibiotic Therapy
Empirical Regimens (pending culture results):
- Antipseudomonal beta-lactams (e.g., ceftazidime, cefepime, piperacillin-tazobactam)
- Carbapenems in multidrug-resistant strains
- Combination with aminoglycosides or fluoroquinolones
Targeted Therapy:
- Adjusted based on sensitivity profiles
- Prolonged IV therapy (4–6 weeks), followed by oral step-down if appropriate
Surgical Intervention
Surgical debridement is often necessary to:
- Remove necrotic tissue and sequestra
- Eliminate biofilm-coated implants or foreign materials
- Drain abscesses
- Provide bone stabilization if required
Reconstructive procedures may involve:
- Bone grafting
- Vascularized tissue transfer
- Negative pressure wound therapy
Chronic Osteomyelitis and Recurrence
Chronic infection by P. aeruginosa is common due to its biofilm resilience and inadequate host clearance. Long-term management includes:
- Repeated debridement
- Suppressive antibiotic regimens in non-operable cases
- Monitoring for complications like pathological fractures or systemic spread
Prognosis and Outcomes
With prompt and aggressive treatment, outcomes can be favorable. However, chronic osteomyelitis carries a risk of recurrence and long-term morbidity. Factors affecting prognosis include:
- Timeliness of diagnosis
- Efficacy of surgical and antibiotic management
- Patient comorbidities
- Pathogen resistance profile
Prevention and Clinical Vigilance
Preventive strategies focus on:
- Rigorous aseptic techniques during surgery
- Prompt management of open fractures
- Early detection of post-operative infections
- Glycemic control in diabetic patients
- Monitoring high-risk populations for early signs of infection
Frequently Asked Questions:
Q1. How is Pseudomonas aeruginosa osteomyelitis diagnosed definitively?
A definitive diagnosis requires a bone biopsy with culture and sensitivity testing to identify the presence of Pseudomonas aeruginosa.
Q2. What makes Pseudomonas osteomyelitis more difficult to treat than other bacterial bone infections?
Its biofilm formation and multidrug resistance mechanisms significantly reduce antibiotic efficacy, necessitating prolonged treatment and often surgical debridement.
Q3. Can Pseudomonas aeruginosa osteomyelitis become chronic?
Yes, if not adequately treated, it frequently progresses to chronic infection due to biofilm protection and delayed immune clearance.
Q4. What is the role of surgery in treating this infection?
Surgery is essential for removing necrotic tissue, draining abscesses, and reducing bacterial load, which facilitates antibiotic effectiveness.
Q5. Are there oral antibiotics effective against Pseudomonas osteomyelitis?
Certain fluoroquinolones like ciprofloxacin may be effective orally, but only after initial IV therapy and based on susceptibility testing.