Pseudomonas aeruginosa joint infection, though less common than those caused by Staphylococcus species, presents a serious clinical challenge, particularly in immunocompromised individuals, post-surgical patients, and intravenous drug users. As an aggressive gram-negative organism, P. aeruginosa has the ability to infiltrate synovial joints, leading to rapid joint destruction if untreated. This article provides a detailed overview of its etiology, risk factors, clinical features, diagnostic approach, treatment strategies, and prognosis.
Pathogenesis of Pseudomonas Aeruginosa Joint Infections
P. aeruginosa invades joints primarily through hematogenous spread or direct inoculation via surgical procedures or trauma. Once established, the bacterium induces an acute inflammatory response in the synovial membrane, leading to cartilage destruction and potential osteomyelitis.
Virulence Mechanisms
- Biofilm formation on prosthetic joints
- Exotoxin production (e.g., ExoS, ExoU)
- Quorum sensing to regulate virulence genes
- Resistance to neutrophil-mediated killing
Risk Factors for Pseudomonal Joint Involvement
- Immunosuppressive therapy or diseases (HIV, diabetes, malignancy)
- Intravenous drug use
- Recent joint surgery or prosthetic joint replacement
- Penetrating trauma or joint injections
- Prolonged hospitalization or intensive care stay
- Prior exposure to broad-spectrum antibiotics
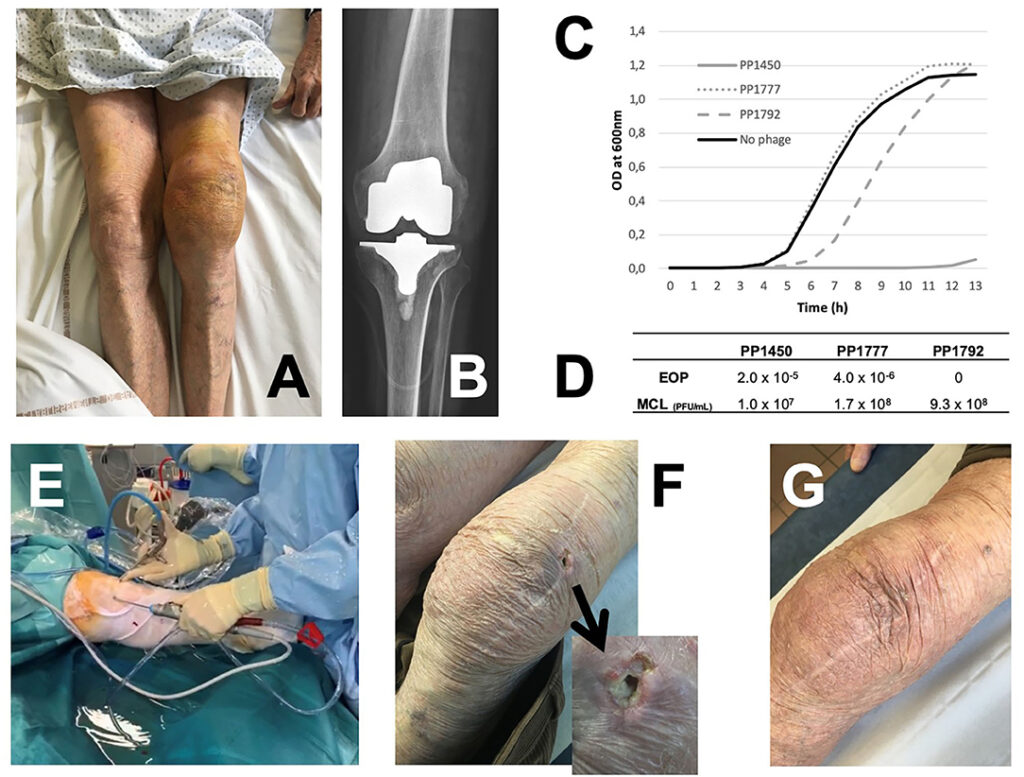
Clinical Presentation of Pseudomonas-Induced Septic Arthritis
Patients with P. aeruginosa joint infections typically present acutely with:
- Severe joint pain, swelling, and erythema
- Restricted range of motion
- Fever and malaise
- Warmth and tenderness over the affected joint
- Common sites: knee, hip, shoulder, and ankle
In prosthetic joint infections, symptoms may be more indolent, with signs of implant loosening or sinus tract formation.
Diagnostic Strategies for Joint Infections Caused by Pseudomonas
Timely and accurate diagnosis is critical to prevent irreversible joint damage.
Key Investigations
- Arthrocentesis: Synovial fluid analysis (WBC >50,000/mm³, PMN predominance, low glucose)
- Gram Stain and Culture: Identifies P. aeruginosa and antibiotic sensitivities
- Blood Cultures: Positive in hematogenous spread
- Imaging:
- X-ray: Joint space narrowing, erosions (late)
- Ultrasound/MRI: Joint effusion, early synovial inflammation
- Molecular diagnostics: PCR for rapid detection and resistance markers
Treatment of Pseudomonas Aeruginosa Septic Arthritis
Treatment requires a multidisciplinary approach involving infectious disease specialists, orthopedic surgeons, and rehabilitation teams.
Empiric and Targeted Antibiotic Therapy
Initial broad-spectrum coverage is narrowed once sensitivities are available.
- Antipseudomonal Beta-Lactams: Cefepime, Piperacillin-tazobactam
- Carbapenems: Meropenem (for ESBL producers)
- Fluoroquinolones: Ciprofloxacin (oral step-down in susceptible strains)
- Aminoglycosides: Amikacin (as adjunct)
- Newer agents: Ceftolozane-tazobactam for resistant strains
Duration:
- Native joint: 3–4 weeks IV antibiotics
- Prosthetic joint: 6 weeks IV + possible suppressive therapy if retained
Surgical Interventions
- Joint Aspiration or Arthroscopic Lavage: Early cases without abscess or implant
- Open Surgical Debridement: For purulent collections, prosthetic infection
- Two-Stage Prosthesis Exchange: Gold standard in chronic prosthetic joint infection
- Joint Fusion or Excision Arthroplasty: Salvage options for non-reconstructable joints
Prognosis and Outcomes
Prognosis depends on:
- Promptness of diagnosis and treatment
- Patient’s immune status and comorbidities
- Virulence and resistance of the infecting strain
- Presence and management of prosthetic material
Early and aggressive treatment generally leads to full recovery of joint function. Delay in intervention can result in permanent disability, chronic pain, or systemic spread (e.g., osteomyelitis or sepsis).
Prevention Strategies in Healthcare Settings
- Strict aseptic technique during joint procedures
- Prophylactic antibiotics for high-risk surgeries
- Prompt removal or replacement of infected prosthetic joints
- Minimizing catheter-related bloodstream infections
- Surveillance for multidrug-resistant organisms (MDROs)
Pseudomonas aeruginosa joint infections, though rare, are clinically significant due to their potential to cause rapid joint destruction, resistance to standard antibiotics, and high morbidity in vulnerable populations. A comprehensive and coordinated approach that integrates microbiological precision, timely surgical intervention, and tailored antibiotic therapy is imperative for optimal patient outcomes.