Pseudomonas aeruginosa infection is a significant cause of healthcare-associated morbidity due to its adaptability, resistance mechanisms, and broad clinical spectrum. As a formidable opportunistic pathogen, it affects immunocompromised patients, those with invasive devices, and individuals with chronic illnesses. This article provides a comprehensive overview of the epidemiology, pathophysiology, clinical manifestations, diagnosis, treatment, and prevention of P. aeruginosa infections.
Understanding Pseudomonas Aeruginosa: A Resilient Pathogen
P. aeruginosa is a gram-negative, aerobic rod-shaped bacterium found ubiquitously in soil, water, and hospital environments. Its intrinsic resistance to many antibiotics and its ability to acquire additional resistance genes make it a challenging pathogen in clinical settings.
Key Microbiological Traits
- Non-lactose fermenting
- Motile with polar flagella
- Produces pigments like pyocyanin and pyoverdine
- Capable of biofilm formation on tissues and medical devices
Routes and Risk Factors of Pseudomonas Aeruginosa Infection
Common Transmission Pathways
- Direct contact with contaminated surfaces or fluids
- Hospital devices such as ventilators, catheters, or IV lines
- Open wounds, especially burns
- Aspiration in intubated patients
High-Risk Populations
- ICU patients with prolonged hospitalization
- Immunocompromised individuals (e.g., cancer, transplant, HIV)
- Cystic fibrosis patients
- Individuals with chronic wounds or diabetes
- Patients with prior broad-spectrum antibiotic exposure
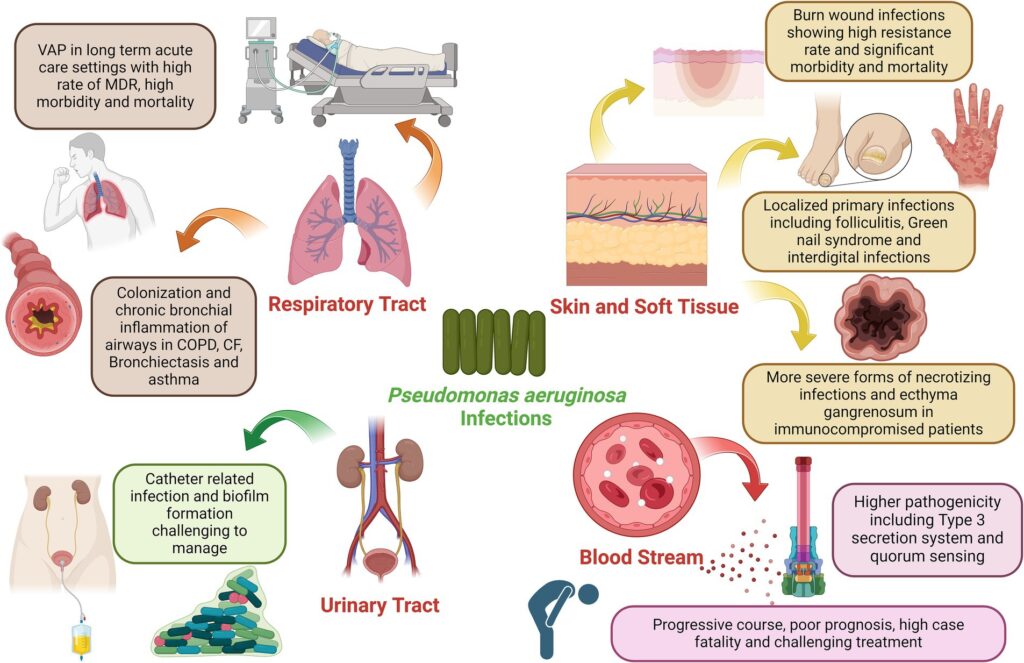
Clinical Manifestations by System
P. aeruginosa can cause both localized and systemic infections. Its clinical presentations vary based on the site of entry and host factors.
1. Respiratory Infections
- Ventilator-associated pneumonia (VAP)
- Chronic lung infection in cystic fibrosis
- Symptoms: cough, purulent sputum, fever, hypoxia
2. Urinary Tract Infections
- Especially in catheterized patients
- Symptoms: dysuria, fever, foul-smelling urine
3. Wound and Burn Infections
- Delayed healing, greenish pus, necrosis
- Can progress to sepsis if untreated
4. Bacteremia and Sepsis
- Rapid systemic spread
- High mortality without prompt intervention
5. Otitis Externa (Swimmer’s Ear)
- Particularly in humid environments
- Severe cases can lead to malignant otitis externa in diabetics
Infection Mechanisms and Resistance Development
P. aeruginosa uses several virulence factors including exotoxin A, elastases, and Type III secretion systems. Resistance is driven by efflux pumps, beta-lactamase production, and decreased membrane permeability.
Diagnostic Techniques for Pseudomonas Aeruginosa
Accurate diagnosis is crucial for guiding effective treatment. Key methods include:
- Culture and Sensitivity Testing: Identification from sputum, urine, blood, or wound swabs
- Gram Stain: Shows gram-negative rods
- Molecular Testing: PCR to detect resistance genes
- Imaging: Chest X-rays for pneumonia, CT for abscesses
Treatment Strategies: Combating a Multidrug-Resistant Organism
First-Line Antibiotics
Empirical therapy should be guided by local resistance patterns and adjusted based on culture results.
- Piperacillin-tazobactam
- Cefepime
- Meropenem or Imipenem
- Ciprofloxacin (if susceptible)
- Amikacin or Gentamicin
For MDR/XDR Strains
- Ceftolozane-tazobactam
- Ceftazidime-avibactam
- Polymyxins (e.g., colistin)
- Combination therapy may improve outcomes in severe infections
Prevention and Infection Control Measures
Preventing P. aeruginosa infections is crucial, especially in hospitals.
- Hand hygiene compliance among healthcare workers
- Sterile techniques during catheter and line insertions
- Environmental cleaning and disinfection
- Antibiotic stewardship programs
- Surveillance in high-risk units like ICUs
Prognosis and Long-Term Outlook
The prognosis depends on the infection site, patient health, and timeliness of treatment. Complications may include:
- Sepsis and organ failure
- Chronic respiratory infection in CF
- Recurrent UTIs or wound infections
- Prolonged hospital stays and increased mortality in MDR cases
Pseudomonas aeruginosa remains a leading cause of nosocomial and opportunistic infections, particularly in vulnerable patient populations. Early diagnosis, targeted antibiotic therapy, and rigorous infection control are essential to reduce the burden of this adaptable and often drug-resistant pathogen. A coordinated approach involving microbiology, infectious disease specialists, and frontline healthcare workers is vital to improving outcomes.