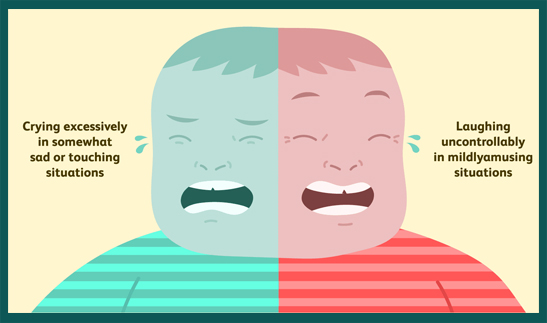
Pseudobulbar affect (PBA) is a neurological disorder characterized by sudden, involuntary episodes of laughing or crying that are disproportionate or unrelated to the individual’s actual emotional state. It is frequently misdiagnosed due to its overlap with mood disorders but remains a distinct clinical condition with a well-established neurological basis.
Defining Pseudobulbar Affect: Clinical Profile and Diagnostic Criteria
Pseudobulbar affect is also known by several other names, including emotional incontinence, pathological laughing and crying (PLC), and involuntary emotional expression disorder (IEED). It arises due to dysfunction in the neural pathways that regulate emotional expression, often secondary to brain injury or disease.
Key Clinical Features
- Involuntary laughing or crying episodes
- Mismatch between emotional expression and internal mood
- Sudden onset, often without a clear trigger
- Brief episodes that resolve quickly
Diagnostic Tools
- Center for Neurologic Study-Lability Scale (CNS-LS)
- Structured interviews and patient history
- Exclusion of mood disorders such as depression or bipolar disorder
Causes and Risk Factors of Pseudobulbar Affect
PBA typically arises secondary to neurological conditions that affect brain regions responsible for emotional regulation, including the prefrontal cortex, brainstem, and cerebellum.
Neurological Conditions Associated with PBA
- Amyotrophic lateral sclerosis (ALS)
- Multiple sclerosis (MS)
- Parkinson’s disease
- Traumatic brain injury (TBI)
- Stroke
- Alzheimer’s disease and other dementias
Pathophysiological Mechanism
Damage to the corticobulbar tract and related neural circuits leads to disinhibition of motor pathways that control emotional expression, resulting in unregulated outbursts of laughter or crying.
Differentiating PBA from Mood Disorders
Although pseudobulbar affect is often confused with depression, especially due to crying episodes, it is essential to distinguish between the two.
| Feature | Pseudobulbar Affect | Depression |
|---|---|---|
| Duration of episodes | Seconds to minutes | Weeks or months |
| Emotional congruence | Incongruent with internal mood | Congruent with mood |
| Trigger | May occur without clear trigger | Triggered by life events |
| Mood symptoms | Not persistently low mood | Persistent sadness, anhedonia |
Pseudobulbar Affect Symptoms and Impact on Quality of Life
The hallmark symptoms of PBA include:
- Sudden and frequent crying or laughing
- Minimal or absent emotional trigger
- Impairment in social, occupational, and interpersonal function
- Embarrassment, frustration, or social withdrawal due to symptoms
These symptoms can significantly degrade the quality of life, especially if misdiagnosed and untreated.
Diagnosis and Evaluation: Steps Toward Accurate Identification
Proper diagnosis requires a multidisciplinary approach, incorporating neurology, psychiatry, and neuropsychology.
Steps in Diagnostic Evaluation
- Detailed patient history and symptom chronology
- Neurological assessment for underlying conditions
- Use of validated screening tools (CNS-LS)
- Neuroimaging if needed (MRI, CT)
- Exclusion of psychiatric causes
Early recognition is critical to avoid misdiagnosis and initiate appropriate treatment.
Treatment Options for Pseudobulbar Affect
The management of PBA involves pharmacologic and non-pharmacologic strategies aimed at symptom control and improving life quality.
FDA-Approved Treatment
- Dextromethorphan-quinidine (Nuedexta)
The only FDA-approved medication for PBA, this combination modulates glutamate signaling and serotonin reuptake to stabilize emotional expression.
Off-Label Medications
- Antidepressants
- SSRIs (e.g., fluoxetine, sertraline)
- TCAs (e.g., amitriptyline, nortriptyline) These are used for their serotonergic activity, though not specifically approved for PBA.
Supportive Therapies
- Cognitive-behavioral therapy (CBT)
- Patient and caregiver education
- Support groups and psychosocial support
Living with Pseudobulbar Affect: Coping Strategies and Lifestyle Tips
While pharmacotherapy is central, supportive strategies enhance outcomes and day-to-day coping.
Practical Recommendations
- Open communication with family and coworkers about the condition
- Identifying triggers and practicing mindfulness or breathing techniques
- Maintaining social activities to prevent isolation
- Using humor cautiously, as it can inadvertently trigger episodes
Research and Future Directions
Emerging therapies target specific neurotransmitter pathways and neuromodulation techniques such as transcranial magnetic stimulation (TMS) are being explored. Further clinical trials and biomarker studies aim to improve diagnostic precision and therapeutic efficacy.
Pseudobulbar affect is a distinct, often underdiagnosed neurological disorder that profoundly affects emotional expression and social functioning. Through proper diagnosis and the use of targeted therapies like dextromethorphan-quinidine, patients can experience significant symptom relief and improved quality of life. A multidisciplinary and compassionate approach remains key to successful management.

