Pruritus, or chronic itching of the skin, is a frequent dermatological and systemic complaint that significantly affects patient well-being. It may occur as a standalone symptom or be indicative of underlying dermatologic, neurologic, systemic, or psychogenic conditions. A precise understanding of the etiology and pathophysiology is crucial for effective treatment.

Defining Pruritus: Clinical Presentation and Classification
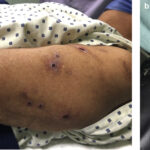
Pruritus is defined as an unpleasant sensation that provokes the urge to scratch. It may be acute (less than 6 weeks) or chronic (lasting longer than 6 weeks). Clinically, it can present with or without visible skin lesions.
Types of Pruritus Based on Etiology
- Dermatologic pruritus: Associated with conditions like eczema, psoriasis, and scabies
- Systemic pruritus: Linked to chronic kidney disease, liver disease, and thyroid disorders
- Neuropathic pruritus: Due to nerve damage, as in multiple sclerosis or notalgia paresthetica
- Psychogenic pruritus: Arising from psychiatric disorders like anxiety or OCD
- Idiopathic pruritus: When no underlying cause is identified
Common Causes of Chronic Skin Pruritus
Understanding the underlying cause is essential for management. Major causes include:
Dermatological Conditions
- Atopic dermatitis
- Contact dermatitis
- Psoriasis
- Urticaria
- Scabies or lice infestation
Systemic Disorders
- Chronic kidney disease (uremic pruritus)
- Cholestatic liver disease (bile salt accumulation)
- Iron deficiency anemia
- Thyroid dysfunction (hyperthyroidism or hypothyroidism)
- Hematologic malignancies (e.g., Hodgkin lymphoma)
Environmental and Lifestyle Factors
- Dry skin (xerosis), especially in elderly individuals
- Heat and sweat
- Allergens or irritants in soaps, cosmetics, or fabrics
Pathophysiology of Pruritus: How Itching Occurs
Pruritus involves a complex interaction between peripheral sensory nerves, skin cells, immune mediators, and the central nervous system.
Key mediators include histamine, interleukin-31 (IL-31), proteases, and neuropeptides like substance P.
Clinical Evaluation: Diagnostic Approach to Pruritus
A comprehensive evaluation includes:
Patient History
- Duration, location, and timing of itch
- Associated symptoms: rash, weight loss, fever
- Personal or family history of skin or systemic diseases
Physical Examination
- Inspection of skin: primary or secondary lesions, excoriations, lichenification
- Lymphadenopathy or organomegaly if systemic etiology is suspected
Laboratory and Diagnostic Tests
- CBC: Rule out anemia or hematologic malignancies
- Liver and renal function tests
- Thyroid profile
- Skin biopsy if diagnosis is unclear
- Chest X-ray or CT: If paraneoplastic pruritus is suspected
Treatment of Pruritus: A Multi-Pronged Approach
1. General Skin Care
- Regular use of moisturizers, especially emollients with ceramides
- Avoid hot showers and use mild, fragrance-free soaps
- Keep ambient air cool and humidified
2. Topical Therapies
- Topical corticosteroids: For inflammatory dermatoses
- Calamine lotion and pramoxine: Provide soothing effect
- Topical capsaicin: For neuropathic itch
3. Systemic Medications
- Antihistamines (e.g., hydroxyzine, cetirizine): For histamine-mediated itching
- Gabapentin or pregabalin: For neuropathic pruritus
- SSRIs or mirtazapine: Useful in psychogenic or refractory cases
- Opioid receptor modulators (e.g., nalfurafine): For uremic or cholestatic pruritus
4. Phototherapy
- Narrow-band ultraviolet B (NB-UVB) therapy effective in chronic pruritus of various origins
Pruritus and Quality of Life
Persistent itch can severely impair sleep, daily functioning, and emotional well-being. Patients may experience:
- Insomnia
- Anxiety and depression
- Social withdrawal
Management must incorporate psychosocial support alongside medical therapy.
When to Refer
Referral to specialists is indicated when:
- Pruritus is unresponsive to initial treatment
- Underlying systemic illness is suspected
- Skin biopsy or further imaging is needed
- Psychiatric evaluation is warranted for psychogenic pruritus
Pruritus of the skin is a complex symptom with a wide differential diagnosis. A patient-centered, methodical approach that considers dermatological, systemic, and psychosocial factors is essential. Emerging insights into neuroimmune pathways and targeted therapies are enhancing our ability to manage even the most challenging cases of chronic itch.