Pruritus, commonly referred to as itching, is a highly prevalent and distressing symptom in patients with end-stage renal disease (ESRD) undergoing hemodialysis. Known as uremic pruritus, this condition is underrecognized despite its significant impact on quality of life, sleep, and morbidity. A systematic, pathophysiologically informed approach to diagnosis and treatment is essential in managing pruritus in hemodialysis-dependent chronic kidney disease (CKD).
Epidemiology of Pruritus in Hemodialysis Patients
Chronic pruritus affects nearly 40% to 50% of patients on maintenance hemodialysis. Prevalence varies with dialysis modality, treatment adequacy, and regional practices.
Key Statistics
- Higher prevalence in males and older adults
- Associated with longer dialysis duration
- Strong correlation with increased mortality and depression
Pathophysiology: Mechanisms Underlying Uremic Pruritus
The pathogenesis of pruritus in CKD is multifactorial and not completely elucidated, involving complex interactions among systemic inflammation, immune dysregulation, and metabolic imbalances.
Contributing Factors
- Hyperparathyroidism: Increases calcium-phosphate product, leading to skin calcification
- Uremic toxins: Accumulation of pruritogens such as β2-microglobulin
- Mast cell activation: Triggers histamine-independent itch
- Xerosis: Dry skin due to reduced sweat gland activity
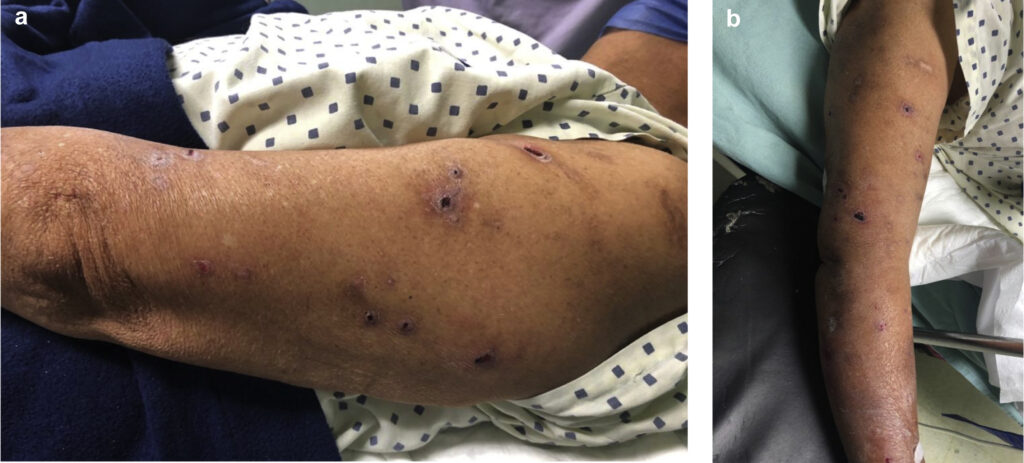
Clinical Manifestations of Hemodialysis-Associated Pruritus
Pruritus in CKD is often:
- Bilateral and symmetric
- Most intense on back, arms, and face
- Worse at night, interfering with sleep
- May lead to excoriations, lichenification, and secondary infections
Psychological sequelae include anxiety, depression, and decreased health-related quality of life.
Diagnostic Considerations and Differential Diagnosis
Diagnosis is clinical and based on:
- History of chronic renal failure and hemodialysis
- Exclusion of other dermatologic conditions (e.g., eczema, scabies, psoriasis)
- Evaluation of serum calcium, phosphate, PTH, and urea levels
It is critical to exclude hepatic, hematologic, or allergic causes of itching in advanced renal disease.
Treatment Strategies for CKD-Related Pruritus
1. Optimize Dialysis Adequacy
- Ensure proper dialysis clearance (Kt/V > 1.2)
- Consider switching to high-flux membranes or hemodiafiltration
2. Skin Care Measures
- Emollients: Intensive moisturizers to treat xerosis
- Topical capsaicin or pramoxine: Target nerve endings to reduce itch
3. Pharmacologic Therapies
- Gabapentin or pregabalin: Reduce neuropathic itch
- Nalfurafine: A kappa-opioid receptor agonist approved in Japan
- Antihistamines: Often ineffective alone but may aid sleep
- Antidepressants (mirtazapine, sertraline): Address both pruritus and mood disturbances
4. Phototherapy
- Narrow-band UVB (NB-UVB): Effective for patients with refractory symptoms
- Mechanism involves modulation of skin immune cells and nerve fibers
5. Novel and Emerging Therapies
- Difelikefalin: Recently approved kappa-opioid receptor agonist showing significant efficacy in large trials
- Charcoal hemoperfusion: Experimental technique to remove circulating pruritogens
Multidisciplinary Management and Quality of Life Enhancement
Successful treatment requires:
- Nephrologists, dermatologists, and mental health professionals
- Regular screening using tools such as the 5-D Itch Scale or Visual Analog Scale (VAS)
- Sleep hygiene, psychological support, and patient education
Prognosis and Long-Term Outlook
Although pruritus in dialysis patients is rarely life-threatening, it is linked with:
- Increased all-cause mortality
- Reduced dialysis adherence
- Higher hospitalization rates
Effective symptom management directly improves patient retention, mood, and compliance with care protocols.
Pruritus in hemodialysis-dependent chronic kidney disease is a complex, multifactorial, and often underappreciated clinical challenge. By recognizing its pathophysiological underpinnings and implementing a tailored, evidence-based treatment strategy, healthcare providers can significantly enhance the well-being and quality of life for affected individuals. Ongoing research into novel therapeutics such as kappa-opioid receptor modulators holds promise for more effective and targeted relief in the near future.

