Pruritus ani is defined as an unpleasant sensation of itching localized to the perianal area, often resulting in an irresistible urge to scratch. This condition, though often underestimated, can significantly impair quality of life and poses a diagnostic challenge due to its multifactorial etiology.
Understanding Pruritus Ani: Pathophysiology and Etiologic Factors
Primary vs. Secondary Pruritus Ani
- Primary (idiopathic): No identifiable underlying cause. Often associated with dermatological sensitivity or hygiene habits.
- Secondary: Attributable to identifiable local or systemic causes including infections, dermatologic diseases, anorectal conditions, and systemic illnesses.
Common Causes of Secondary Pruritus Ani
Dermatologic Conditions
- Contact dermatitis: Reaction to soaps, wipes, topical medications
- Psoriasis or lichen planus: Chronic inflammatory skin disorders
- Seborrheic dermatitis: Especially in immunocompromised patients
Infections
- Candidiasis: Common in diabetics and immunosuppressed
- Pinworms (Enterobius vermicularis): Frequently affects children and their caregivers
- Bacterial overgrowth: Poor hygiene or incontinence may contribute
Anorectal Diseases
- Hemorrhoids
- Anal fissures
- Fistulas and abscesses
- Fecal soiling: Residual stool causing irritation
Systemic Conditions
- Diabetes mellitus
- Renal failure
- Liver disease with cholestasis
- HIV infection
Clinical Presentation and Symptoms
Patients commonly report:
- Persistent or intermittent anal itching, worse at night or after defecation
- Associated burning, soreness, or redness
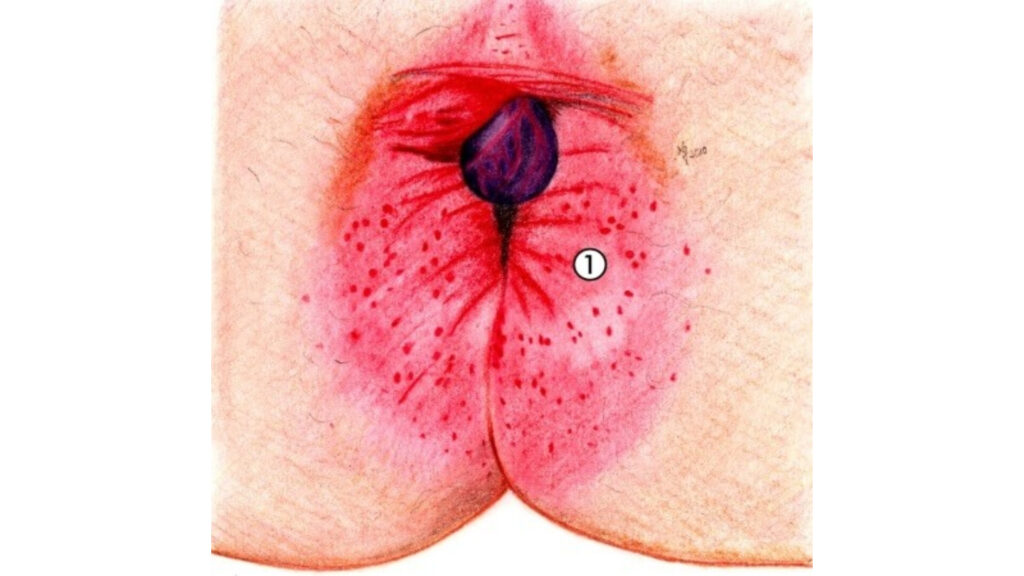
- Evidence of excoriations, lichenification, or perianal eczema upon examination
Severe scratching may result in secondary infection and thickening of the perianal skin, creating a chronic itch-scratch cycle.
Diagnostic Evaluation of Anal Pruritus
Clinical History
A detailed history is essential, focusing on:
- Onset and duration
- Hygiene habits
- Topical agents used
- Associated systemic symptoms
- Family or sexual history of infections
Physical Examination
- Inspection of the perianal region for inflammation, rashes, lesions, or incontinence-related changes
- Anoscopic examination to evaluate internal hemorrhoids or fissures
Diagnostic Tests
- Stool examination: Ova and parasites (especially in children)
- Skin scrapings: For fungal infections
- Patch testing: If allergic contact dermatitis is suspected
- Biopsy: Rarely needed, for persistent or atypical cases
Differential Diagnosis
| Condition | Differentiating Features |
|---|---|
| Hemorrhoids | Bright red blood, palpable masses |
| Contact dermatitis | History of irritant or allergen exposure |
| Psoriasis | Silvery scales, often with systemic involvement |
| Fungal infection | Satellite lesions, positive KOH test |
| Lichen sclerosus | White plaques, commonly in postmenopausal women |
| Pinworm infestation | Nocturnal itching, especially in children |
Management and Treatment of Pruritus Ani
General Measures
- Gentle hygiene: Use lukewarm water without soap, pat dry gently
- Avoid irritants: Fragranced wipes, soaps, or over-the-counter creams
- Loose-fitting cotton underwear: Reduces friction and allows ventilation
- Barrier creams: Zinc oxide or petroleum jelly for skin protection
Topical Therapies
- Mild topical corticosteroids: Hydrocortisone 1% for short-term relief
- Antifungal creams: Clotrimazole or miconazole for suspected candidiasis
- Capsaicin cream: In chronic cases to desensitize nerve endings
- Topical calcineurin inhibitors: For steroid-sparing long-term control
Systemic Therapies
- Oral antihistamines: Nighttime use for itch relief
- Antibiotics or antifungals: For confirmed infections
- Antihelminthic agents: Albendazole or mebendazole for pinworms
Chronic Pruritus Ani: Advanced Interventions
- Botulinum toxin injection: Off-label use for severe, treatment-resistant cases
- Psychological support: For patients with obsessive scratching or psychogenic causes
- Referral to dermatology or colorectal surgery: For persistent or complicated cases
Prognosis and Patient Outcomes
With proper diagnosis and individualized treatment, the majority of patients experience significant improvement. However, recurrence is common if underlying causes are not adequately managed or hygiene practices remain unchanged.
Preventive Strategies and Patient Education
- Regular and non-irritating hygiene
- Avoidance of unnecessary topical medications
- Dietary adjustments to prevent constipation or diarrhea
- Timely treatment of underlying anorectal or dermatological conditions
Pruritus ani, though common, warrants careful evaluation to identify underlying causes and tailor appropriate management. A multidisciplinary approach combining dermatologic, proctologic, and patient-centered strategies ensures optimal outcomes and reduced recurrence. With advances in both topical and systemic therapies, clinicians are better equipped than ever to address this often distressing condition effectively.

