Proteus pneumonia is an infrequent but clinically significant infection of the lower respiratory tract caused by Proteus species, predominantly Proteus mirabilis. Typically affecting immunocompromised individuals or those with prolonged hospital stays, this gram-negative pneumonia is associated with high morbidity and requires early identification and targeted treatment for optimal outcomes.
Microbiological Insights into Proteus Species
Characteristics and Respiratory Pathogenicity
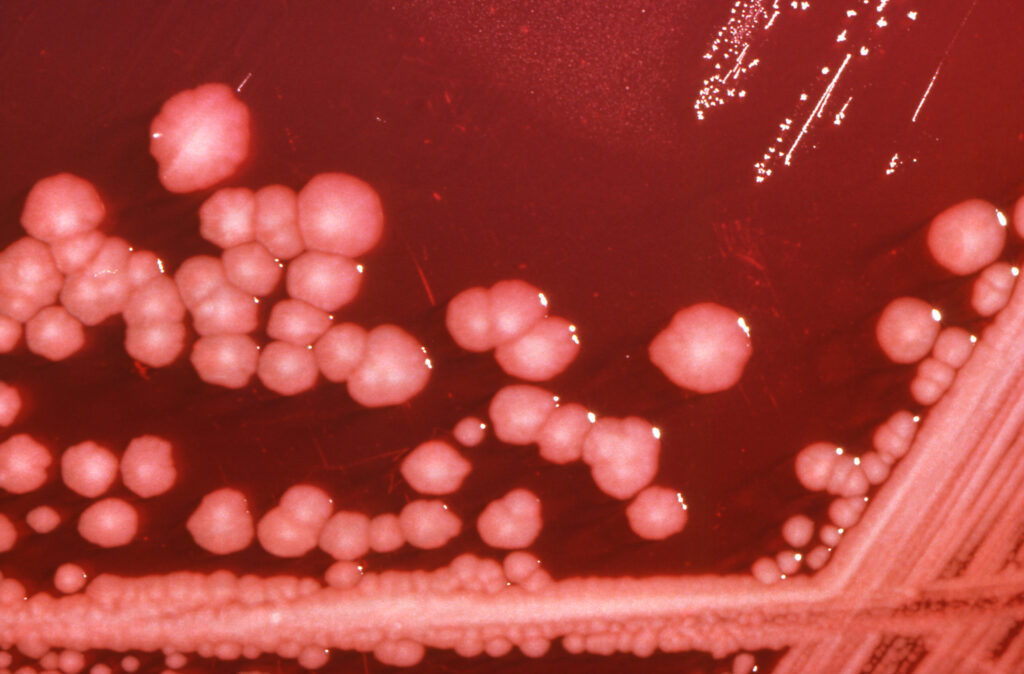
Proteus species are gram-negative, facultatively anaerobic bacilli from the Enterobacteriaceae family. While commonly implicated in urinary tract infections and wound infections, pulmonary involvement is rare and usually nosocomial in origin.
Key features include:
- Motility: Facilitates movement into deeper lung tissues.
- Urease production: Alters the microenvironment, aiding colonization.
- Biofilm formation: Promotes persistence on ventilator surfaces and catheters.
- Multidrug resistance: Complicates empirical treatment.
These organisms may colonize the oropharynx, especially in patients with prolonged intubation, leading to aspiration and subsequent pulmonary infection.
Epidemiology and Risk Factors
Patient Populations at Risk
Proteus pneumonia predominantly affects hospitalized or immunosuppressed patients. Major risk factors include:
- Mechanical ventilation
- Chronic obstructive pulmonary disease (COPD)
- Aspiration risk due to altered mental status
- Diabetes mellitus
- Prolonged antibiotic use
- Neoplastic diseases
- Recent abdominal or thoracic surgery
This infection is often a manifestation of ventilator-associated pneumonia (VAP) or secondary pneumonia in patients with complex comorbidities.
Clinical Manifestations of Proteus-Induced Pneumonia
Symptoms and Physical Examination Findings
Symptoms of Proteus pneumonia closely resemble those of other bacterial pneumonias but may be more severe due to underlying host factors:
- High-grade fever and chills
- Productive cough with purulent or blood-streaked sputum
- Dyspnea and tachypnea
- Chest pain, particularly pleuritic in nature
- Auscultatory findings: rales, bronchial breath sounds, or dullness to percussion
- Cyanosis and hypoxia in advanced stages
In critical cases, systemic sepsis or acute respiratory distress syndrome (ARDS) may ensue.
Diagnostic Workup
Laboratory and Radiologic Evaluation
An integrated diagnostic approach is essential for definitive identification and appropriate management.
- Sputum analysis: Reveals gram-negative rods and abundant neutrophils.
- Culture and sensitivity: Confirm species and guide targeted therapy.
- Chest imaging: Shows consolidation, cavitation, or bilateral infiltrates.
- Blood cultures: Important for detecting bacteremia or septic progression.
- Bronchoscopy: Occasionally warranted in ventilated patients or non-resolving cases.
Antimicrobial Therapy and Clinical Management
Empirical and Directed Treatment Options
Due to the resistance potential of Proteus, empirical therapy must be promptly initiated and refined based on culture reports.
- Empirical therapy:
- Piperacillin-tazobactam
- Cefepime or meropenem in severe cases
- Targeted therapy (based on susceptibility):
- Ceftriaxone, ciprofloxacin, or gentamicin
- Avoid ampicillin in resistant strains
- Duration: 10–14 days, extended in complicated or slow-resolving infections
Supportive and Adjunctive Measures
- Oxygen supplementation or mechanical ventilation as needed
- Fluid and electrolyte correction
- Antipyretics and bronchodilators
- Airway clearance techniques (e.g., chest physiotherapy)
- Discontinuation or rotation of unnecessary antibiotics to prevent resistance
Complications and Prognosis
Adverse Outcomes and Long-Term Risks
Delayed diagnosis or inadequate treatment may lead to:
- Pulmonary abscess or necrosis
- Septicemia and multiorgan dysfunction
- Empyema requiring drainage
- Prolonged ventilator dependence
- Chronic respiratory insufficiency
Prognosis largely depends on the timeliness of intervention, underlying health status, and presence of complications.
Prevention and Infection Control Strategies
Reducing Incidence in Healthcare Settings
Hospitals should implement strict preventive measures, particularly in intensive care units:
- Rigorous hand hygiene and use of personal protective equipment
- Strict ventilator care bundles to prevent VAP
- Timely de-escalation of antibiotics
- Regular oral care for intubated patients
- Early mobilization and pulmonary hygiene
Antimicrobial stewardship programs are pivotal in reducing the emergence of resistant Proteus strains.
Proteus pneumonia, though uncommon, presents a serious threat to hospitalized and immunocompromised individuals. Prompt recognition, accurate microbial diagnosis, and aggressive therapeutic strategies are essential to mitigate the disease’s complications. With vigilant infection control and tailored antibiotic regimens, healthcare providers can improve patient outcomes and curb the impact of this formidable gram-negative pathogen.