Pelvic inflammatory disease (PID) is a serious reproductive health concern characterized by infection of the female upper genital tract. While Neisseria gonorrhoeae and Chlamydia trachomatis are common etiological agents, Proteus mirabilis, a gram-negative facultative anaerobe, has been increasingly recognized in polymicrobial PID, particularly among individuals with underlying urogenital infections. This article provides a comprehensive overview of the clinical significance, diagnostic strategies, and treatment modalities associated with Proteus mirabilis in PID.
Etiological Role of Proteus mirabilis in Pelvic Inflammatory Disease
Microbial Characteristics and Pathogenesis
Proteus mirabilis exhibits virulence factors that facilitate ascending infection from the lower to upper genital tract:
- Urease production: Raises local pH, promoting tissue damage and stone formation in the urinary tract, which can contribute to adjacent reproductive tract infection.
- Fimbriae (e.g., MR/P, PMF): Promote adherence to epithelial cells in the vaginal and uterine environment.
- Motility via flagella: Enhances the organism’s ability to traverse the mucosal surfaces.
- Biofilm formation: Increases resistance to host immunity and antibiotics.
This bacterium’s capacity for persistent colonization makes it a concerning pathogen in cases of recurrent or treatment-resistant PID.
Risk Factors for Proteus-Associated PID
Patient-Specific Risk Enhancers
- Recent urogenital procedures or instrumentation
- History of urinary tract infections, especially recurrent
- Use of intrauterine devices (IUDs)
- Immunosuppression or diabetes mellitus
- Poor genital hygiene
- Polymicrobial vaginal flora imbalances
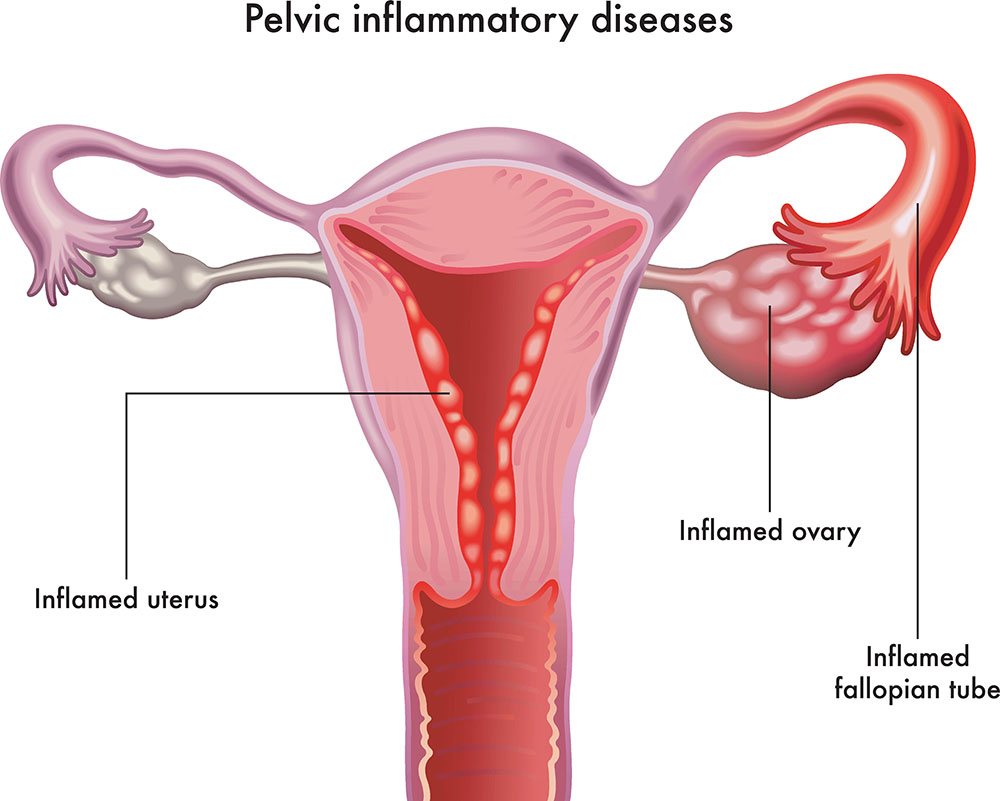
Clinical Presentation and Symptomatology
Distinctive Features of Proteus PID
While the general symptoms of PID may overlap regardless of the causative agent, the following may suggest involvement of Proteus mirabilis:
- Lower abdominal and pelvic pain
- Purulent vaginal discharge with a strong ammonia-like odor
- Dysuria and urinary frequency (coexisting UTI)
- Fever and chills in systemic cases
- Dyspareunia and menstrual irregularities
In severe cases, patients may present with signs of tubo-ovarian abscesses, peritonitis, or septic shock.
Diagnostic Evaluation
Laboratory and Imaging Tools
- Pelvic examination: Reveals cervical motion tenderness, uterine/adnexal tenderness.
- Microbiological cultures: Essential to isolate Proteus mirabilis alongside other flora.
- Urinalysis: Useful in identifying concurrent urinary tract infection.
- Imaging: Indicated if abscesses, free fluid, or anatomical anomalies are suspected.
Antimicrobial Therapy and Treatment Guidelines
Empirical and Targeted Treatment Approaches
Due to the polymicrobial nature of PID, broad-spectrum antibiotic therapy is the standard:
- Initial empiric therapy may include:
- Ceftriaxone (single dose) + Doxycycline (14 days) + Metronidazole (14 days)
- If Proteus mirabilis is isolated, consider:
- Ciprofloxacin or cefepime for targeted gram-negative coverage
- Aminoglycosides (e.g., gentamicin) in inpatient settings
- Duration: Typically 10–14 days, adjusted for severity and patient response
Inpatient Management Indications
- High fever and severe pelvic pain
- Failure of oral therapy
- Tubo-ovarian abscess
- Pregnancy
- Suspected sepsis
Complications of Untreated or Recurrent Proteus PID
Long-Term Reproductive Sequelae
- Infertility: Resulting from fallopian tube scarring and obstruction
- Ectopic pregnancy: Due to tubal damage
- Chronic pelvic pain: A common residual effect
- Perihepatitis (Fitz-Hugh–Curtis syndrome): In rare advanced cases
Early intervention and pathogen-specific treatment are critical in minimizing these risks.
Preventive Strategies and Public Health Considerations
Preventing Ascending Infections
- Regular screening and prompt treatment of UTIs
- Safe sex practices and barrier contraception
- Judicious use and monitoring of IUDs
- Patient education on genital hygiene and symptom awareness
Public health measures focusing on integrated sexual and urological care can reduce incidence rates of Proteus-related PID.
Proteus mirabilis pelvic inflammatory disease, though less common than other bacterial etiologies, demands clinical attention due to its aggressive nature and potential for severe reproductive complications. Accurate diagnosis through microbial identification, guided antimicrobial therapy, and preventive strategies form the cornerstone of effective management. By addressing the urogenital interplay in infections, healthcare providers can enhance outcomes and prevent long-term morbidity in affected women.

