Prosthetic joint infections (PJIs) represent a significant challenge in orthopedic surgery, compromising patient outcomes and increasing healthcare costs. Preventing infections following prosthetic arthroplasty requires a multifaceted approach involving meticulous surgical technique, optimized patient selection, and evidence-based perioperative protocols.
Understanding Prosthetic Joint Infections: Epidemiology and Impact
PJIs occur in approximately 1–2% of primary joint replacements and up to 4% in revision cases. These infections can lead to chronic pain, joint dysfunction, prolonged hospitalization, and even implant removal.
Common pathogens involved:
- Staphylococcus aureus (including MRSA)
- Staphylococcus epidermidis
- Gram-negative bacilli
- Polymicrobial infections in complex cases
Risk Factors Contributing to Infection Post-Arthroplasty
Patient-Related Risk Factors
- Diabetes mellitus
- Obesity (BMI >30)
- Rheumatoid arthritis
- Immunosuppression
- Malnutrition
- Smoking
Surgery-Related Risk Factors
- Prolonged operative time
- Revision surgeries
- Inadequate skin antisepsis
- Suboptimal operating room conditions
Preoperative Infection Prevention Measures
Optimizing Patient Health
- Control of blood glucose levels (target HbA1c < 7%)
- Smoking cessation at least 4 weeks pre-op
- Weight loss and nutritional support
- Screening and decolonization of S. aureus carriers using mupirocin nasal ointment and chlorhexidine washes
Antibiotic Prophylaxis
- First-generation cephalosporins (e.g., cefazolin) administered within 60 minutes prior to incision
- Alternatives for allergies: clindamycin or vancomycin
- Re-dosing during surgery if prolonged or significant blood loss occurs
Intraoperative Strategies for Infection Control
Surgical Technique and Environment
- Minimize operative time and tissue handling
- Maintain strict aseptic technique
- Double gloving and changing outer gloves before prosthesis handling
- Use of sterile body exhaust suits in high-risk environments
Operating Room Protocols
- Laminar airflow systems and HEPA filters
- Limit operating room traffic
- Use of antimicrobial incise drapes
Antiseptic Skin Preparation
- Chlorhexidine-alcohol is superior to povidone-iodine in reducing surgical site infections
Postoperative Care and Monitoring
Wound Management
- Use of occlusive or antimicrobial dressings
- Regular wound inspection and hygiene education
- Avoid unnecessary wound drains unless clinically indicated
Postoperative Antibiotic Stewardship
- Discontinue prophylactic antibiotics within 24 hours
- Prolonged use does not decrease infection rates and may contribute to resistance
Early Detection and Management of Infections
Signs of infection:
- Persistent wound drainage
- Erythema, warmth, or swelling around the joint
- Fever and elevated inflammatory markers (CRP, ESR)
Diagnostic tools:
- Joint aspiration and culture
- Synovial fluid leukocyte count
- Imaging: MRI or labeled leukocyte scans for deep infections
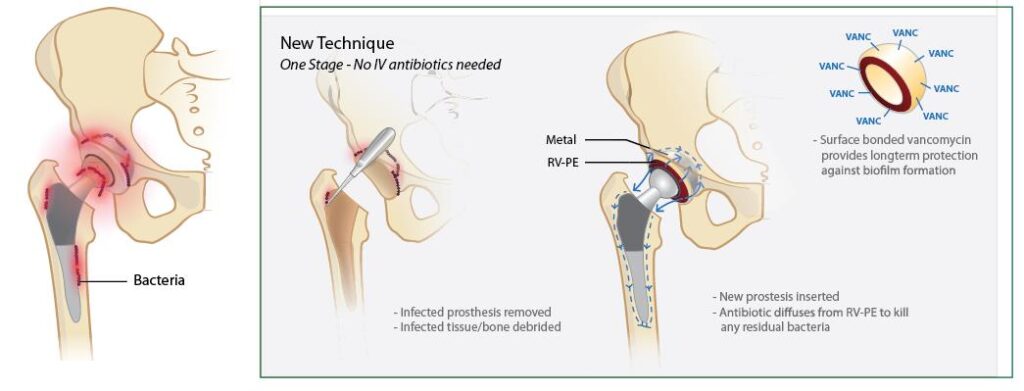
Advanced Prevention Strategies and Innovations
Antibiotic-Loaded Cement
Used in high-risk or revision surgeries, antibiotic-impregnated bone cement can reduce microbial colonization.
Silver-Coated Implants
Silver’s broad-spectrum antimicrobial properties show promise in preventing bacterial adhesion and biofilm formation.
Localized Drug Delivery Systems
Hydrogel coatings and antibiotic-laden sponges placed near the implant offer sustained antimicrobial release.
Personalized Medicine
Genetic screening for infection susceptibility and microbiome modulation are emerging areas of interest.
Preventing infection in prosthetic arthroplasty is critical to ensuring successful surgical outcomes. Through diligent preoperative optimization, rigorous intraoperative protocols, and vigilant postoperative care, the incidence of PJIs can be significantly reduced. Continuous innovation in materials, techniques, and diagnostic tools will further empower clinicians to prevent infections and improve the longevity of prosthetic joints.