Progressive keratoconus is a complex and degenerative eye condition that affects the cornea, leading to visual impairment due to corneal thinning and distortion. This condition gradually worsens over time, causing the cornea to become more conical in shape, which disrupts the normal focusing ability of the eye. The condition can significantly affect an individual’s quality of life, making early detection and effective management essential.
In this article, we will explore the causes, symptoms, diagnostic methods, stages, and treatment options for progressive keratoconus. We will also discuss how advancements in medical technology have led to better outcomes for those living with this condition.
What is Progressive Keratoconus?
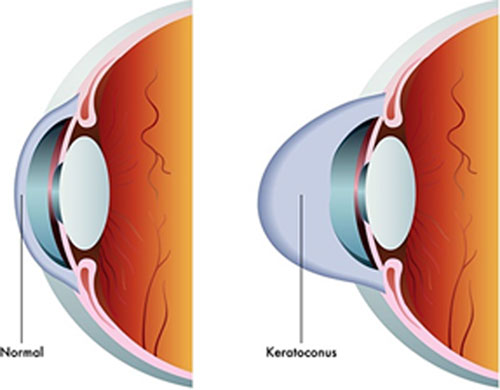
Keratoconus is a progressive condition where the normally round shape of the cornea becomes thinner and bulges outwards, forming a cone-like shape. This irregular shape distorts the way light enters the eye, causing blurred or distorted vision. The condition typically starts during the teenage years or early adulthood and can worsen over time.
While the disease is progressive in nature, it can vary significantly in severity from person to person. Some individuals experience only mild symptoms, while others may face severe vision impairment that requires medical intervention.
Causes and Risk Factors of Progressive Keratoconus
The exact cause of keratoconus remains unknown, but several factors may contribute to its development. Understanding the potential causes and risk factors is crucial for early diagnosis and intervention.
1. Genetic Factors
Genetics plays a significant role in the development of keratoconus. Family history is one of the strongest risk factors, with studies showing that individuals who have close relatives with the condition are at a higher risk. Certain genetic mutations can make individuals more susceptible to corneal weakening, which may result in keratoconus.
2. Environmental and Lifestyle Factors
Chronic eye rubbing is a well-known environmental factor linked to keratoconus. This may cause mechanical damage to the cornea, leading to thinning and distortion over time. Allergies, which often lead to itching and rubbing of the eyes, can exacerbate the condition.
3. Other Eye Conditions
Some conditions, such as Down syndrome, Ehlers-Danlos syndrome, and Leber congenital amaurosis, have been associated with a higher incidence of keratoconus. People with these conditions may have more elastic skin or connective tissues, which may increase the risk of developing corneal thinning.
4. Hormonal Factors
There is evidence to suggest that hormonal changes, particularly during puberty and pregnancy, can influence the development and progression of keratoconus. Many individuals report the worsening of symptoms during periods of significant hormonal changes.
Symptoms of Progressive Keratoconus
The symptoms of progressive keratoconus often begin gradually and worsen over time. Early signs may be subtle, making it important to be aware of potential changes in vision. Common symptoms include:
1. Blurred or Distorted Vision
As the cornea thins and changes shape, the eye loses its ability to focus light properly, resulting in blurred or distorted vision. This symptom often worsens during the later stages of the disease.
2. Increased Sensitivity to Light
People with keratoconus often experience heightened sensitivity to light, known as photophobia. This can make it difficult to drive at night or be in brightly lit environments.
3. Frequent Prescription Changes
Individuals with keratoconus may notice that their vision fluctuates, requiring frequent changes in their eyeglass prescription. This is a common sign of the condition, as the corneal shape continues to change.
4. Halos and Starbursts
Distorted vision can lead to the appearance of halos or starbursts around lights, particularly at night. This can make it difficult to see clearly in low-light conditions.
5. Eye Strain
As the eyes work harder to focus due to the irregular corneal shape, individuals with keratoconus may experience eye strain and discomfort, especially after prolonged periods of reading or using digital devices.
Diagnosing Progressive Keratoconus
Diagnosing keratoconus in its early stages can be challenging due to its gradual progression. However, several diagnostic tests can help healthcare professionals detect the condition.
1. Comprehensive Eye Exam
A thorough eye exam is the first step in diagnosing keratoconus. This includes checking visual acuity, assessing the shape of the cornea, and measuring the thickness of the cornea using a pachymeter.
2. Corneal Topography
Corneal topography is a non-invasive imaging test that creates a detailed map of the cornea’s surface. This test is essential for detecting irregularities in corneal shape, which are characteristic of keratoconus. It can help monitor the progression of the disease over time.
3. Keratometry
Keratometry measures the curvature of the cornea. In individuals with keratoconus, the cornea becomes more cone-shaped, which is detected through this measurement.
4. OCT (Optical Coherence Tomography)
OCT uses light to capture high-resolution images of the cornea, providing valuable information about its structure and thickness. OCT is often used to monitor keratoconus progression and assess the effectiveness of treatments.
Stages of Progressive Keratoconus
Keratoconus progresses through several stages, and the severity of the condition can vary significantly. The stages of progressive keratoconus are typically classified as follows:
1. Mild Stage
In the early stage of keratoconus, the cornea begins to show slight thinning and bulging. Symptoms are usually mild and may include blurred vision or frequent changes in eyeglass prescriptions. Most individuals can manage this stage with corrective lenses or glasses.
2. Moderate Stage
At this stage, the cornea becomes more conical in shape, leading to greater distortion of vision. Patients may experience increased sensitivity to light, halos around lights, and difficulty seeing clearly even with corrective lenses. The condition may require more advanced treatment, such as specialty contact lenses.
3. Advanced Stage
In advanced keratoconus, the cornea becomes severely thin and distorted, leading to significant visual impairment. This stage often requires surgical intervention, such as corneal transplant or crosslinking, to improve vision and prevent further damage.
Treatment Options for Progressive Keratoconus
While there is no cure for progressive keratoconus, various treatment options are available to help manage the condition and preserve vision. The choice of treatment depends on the severity of the disease and the individual’s response to other interventions.
1. Eyeglasses and Contact Lenses
In the early stages of keratoconus, eyeglasses may be sufficient to correct vision. As the disease progresses, however, specialty contact lenses, such as rigid gas-permeable (RGP) lenses, may be required to provide a clearer, more stable image. Scleral lenses are another option that can help in cases of advanced keratoconus.
2. Corneal Crosslinking
Corneal crosslinking is a minimally invasive procedure that strengthens the corneal tissue by using ultraviolet light and riboflavin (vitamin B2). This treatment is effective in halting the progression of keratoconus, particularly in younger patients, and can be used to preserve vision.
3. Intacs
Intacs are small, curved inserts placed into the cornea to help reshape its surface. This treatment is suitable for individuals with moderate keratoconus and can provide significant visual improvement.
4. Corneal Transplant (Keratoplasty)
In cases where other treatments are ineffective, a corneal transplant may be necessary. This involves replacing the damaged cornea with a healthy donor cornea. It is often recommended in advanced stages of keratoconus when vision can no longer be corrected with lenses or crosslinking.
5. Collagen Crosslinking with Topography-Guided PRK
For patients with more advanced keratoconus, combining corneal crosslinking with photorefractive keratectomy (PRK) using a topography-guided approach can improve corneal shape and enhance vision quality.
Prognosis of Progressive Keratoconus
The prognosis for individuals with progressive keratoconus varies depending on the stage of the disease and the effectiveness of treatment. Early detection and management of the condition can help slow its progression and preserve vision for many years. However, in severe cases, vision may deteriorate significantly, requiring surgical interventions like corneal transplantation.
In general, individuals with keratoconus who undergo appropriate treatments, such as corneal crosslinking and specialty contact lenses, can maintain functional vision for many years, even as the disease progresses. With advancements in treatment and early intervention, the long-term outlook for individuals with keratoconus has improved significantly.
Progressive keratoconus is a degenerative eye disease that requires careful management to preserve vision and quality of life. Early diagnosis, effective treatment options, and ongoing monitoring are essential to preventing further progression of the condition. With advancements in medical technology and treatment methods, individuals with keratoconus can maintain their vision and lead productive lives. Understanding the symptoms, causes, and treatment options for progressive keratoconus allows patients to make informed decisions about their care and improve their outcomes.