Primary ovarian failure (POF), also known as primary ovarian insufficiency (POI), is a clinical syndrome characterized by the loss of normal ovarian function before the age of 40. It leads to infertility, hypoestrogenism, and elevated gonadotropin levels. While the condition resembles natural menopause, it occurs significantly earlier and may present intermittently rather than being a permanent cessation of function.
Epidemiology and Risk Factors
Prevalence in the Population
Primary ovarian failure affects approximately 1% of women under 40 years of age and 0.1% under 30. It represents a significant contributor to female infertility worldwide.
Contributing Risk Factors
- Genetic abnormalities: Turner syndrome (45,X), fragile X premutation
- Autoimmune disorders: Autoimmune oophoritis, thyroiditis, Addison’s disease
- Iatrogenic causes: Chemotherapy, radiation therapy, surgical removal of ovaries
- Infectious etiologies: Mumps oophoritis
- Environmental toxins: Cigarette smoke, pesticides, industrial chemicals
Pathophysiology of Primary Ovarian Failure
Hormonal Dysregulation
POF is marked by:
- Low estrogen levels
- Elevated follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
- Irregular or absent ovulation
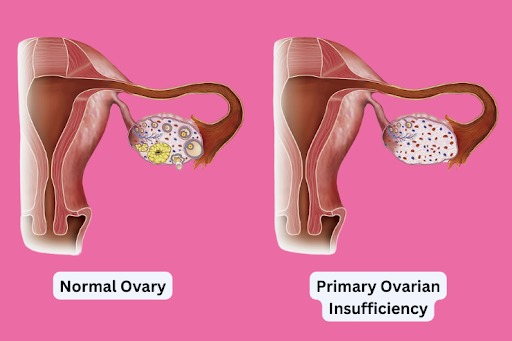
Ovarian Reserve and Follicular Depletion
There is either a complete depletion of primordial follicles or a dysfunction in their maturation and release. Despite high FSH levels, the ovaries fail to respond appropriately, leading to anovulation and hypoestrogenism.
Clinical Presentation and Symptoms
Common Signs and Symptoms
- Amenorrhea or oligomenorrhea
- Infertility
- Hot flashes and night sweats
- Vaginal dryness and dyspareunia
- Mood swings and depression
- Decreased libido
Long-term Complications
- Osteoporosis due to low estrogen
- Increased cardiovascular risk
- Anxiety and psychosocial stress
Diagnostic Criteria and Evaluation
Clinical and Laboratory Evaluation
Diagnosis is established based on:
- Amenorrhea or oligomenorrhea for 4–6 months
- Two elevated serum FSH levels (>40 IU/L), obtained at least one month apart
- Low estradiol levels
Additional Testing
- Karyotype analysis: To detect chromosomal anomalies such as Turner syndrome
- FMR1 gene testing: Screening for fragile X premutation
- Autoimmune panel: To assess for thyroid or adrenal autoimmunity
- Pelvic ultrasound: To evaluate ovarian size and antral follicle count
Differential Diagnosis
Conditions to Exclude
- Hypothalamic amenorrhea (low FSH)
- Polycystic ovary syndrome (PCOS)
- Hyperprolactinemia
- Functional hypothalamic amenorrhea due to stress, excessive exercise, or weight loss
Treatment and Management Options
Hormone Replacement Therapy (HRT)
HRT remains the cornerstone of treatment to restore estrogen levels and protect against osteoporosis and cardiovascular disease. Regimens typically include:
- Estrogen: Transdermal or oral estradiol
- Progestin: To protect the endometrium in women with an intact uterus
Fertility Considerations
While spontaneous ovulation occurs in 5–10% of women with POF, assisted reproductive options are often necessary:
- Egg donation: The most effective fertility treatment
- In vitro fertilization (IVF): With donor or preserved oocytes
- Adoption or surrogacy: Alternative paths to parenthood
Psychosocial Support
Psychological counseling and patient support groups play a vital role in coping with the emotional impact of diagnosis, especially in young women with childbearing aspirations.
Lifestyle and Nutritional Interventions
- Calcium and vitamin D supplementation: To prevent osteoporosis
- Weight-bearing exercise: Enhances bone strength
- Smoking cessation: Protects residual ovarian function
- Stress reduction: Supports hormonal balance
Emerging Therapies and Research Directions
Stem Cell Therapy
Experimental therapies exploring ovarian regeneration using mesenchymal stem cells have shown promise in preliminary studies but remain investigational.
Gene Editing and Hormonal Modulation
Advances in gene therapy and molecular biology may pave the way for personalized medicine approaches to restore ovarian function.
Primary ovarian failure is a multifaceted endocrine disorder requiring a multidisciplinary approach to diagnosis, treatment, and long-term management. Early recognition and timely initiation of hormone replacement therapy are essential to mitigate associated risks, while emerging fertility options provide hope for affected women wishing to conceive. With continued advancements in reproductive medicine and genetics, the landscape of POF management continues to evolve toward more personalized and effective solutions.