Primary hypogonadism is defined as testicular failure that results in inadequate production of testosterone and impaired spermatogenesis. When the etiology is orchitis—an inflammatory condition of the testes—testicular tissue may be permanently damaged, leading to irreversible endocrine and reproductive dysfunction. The condition necessitates early recognition, targeted treatment, and long-term hormonal management to maintain quality of life and metabolic balance.
Understanding Orchitis and Its Impact on Testicular Function
What Is Orchitis?
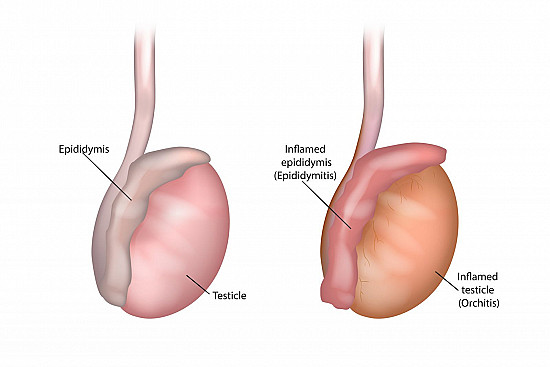
Orchitis refers to inflammation of one or both testicles, most commonly caused by viral or bacterial infections. Viral orchitis is most frequently associated with mumps virus, especially when contracted after puberty. Bacterial causes often result from epididymo-orchitis due to urinary tract infections or sexually transmitted pathogens.
Mechanism of Damage Leading to Hypogonadism
Inflammation can cause testicular edema, interstitial fibrosis, and destruction of seminiferous tubules, impairing both Leydig cell function (which produce testosterone) and Sertoli cell function (which support sperm development). This process culminates in hypergonadotropic hypogonadism, where the pituitary attempts to compensate by secreting more luteinizing hormone (LH) and follicle-stimulating hormone (FSH), yet the testes are unable to respond.
Clinical Presentation of Hypogonadism Due to Orchitis
Acute Symptoms of Orchitis
- Testicular pain and swelling
- Fever and systemic symptoms
- Erythema and warmth over the scrotum
- Dysuria and urethral discharge in bacterial cases
Long-Term Sequelae
After resolution of the acute phase, patients may experience:
- Persistent low libido and erectile dysfunction
- Fatigue, muscle mass loss, and mood disturbances
- Infertility due to azoospermia or oligospermia
- Gynecomastia due to hormonal imbalance
Diagnostic Evaluation
Hormonal Profile
- Low serum testosterone
- Elevated LH and FSH confirming primary testicular failure
- Inhibin B may be reduced, reflecting Sertoli cell dysfunction
Imaging and Semen Analysis
- Scrotal ultrasound may reveal testicular atrophy or calcifications
- Semen analysis frequently shows decreased sperm count and motility
Viral and Bacterial Serologies
- Mumps IgM/IgG titers
- STI screening (e.g., chlamydia, gonorrhea, HIV)
- Urinalysis and urine culture to identify uropathogens
Management of Primary Hypogonadism Post-Orchitis
Acute Phase Treatment
- Antiviral therapy for mumps in early stages (supportive care remains the mainstay)
- Antibiotics for bacterial orchitis
- Scrotal support, NSAIDs, and cold compresses
Long-Term Hormonal Replacement
Lifelong testosterone replacement therapy (TRT) is often required in confirmed hypogonadism:
- Injectables: testosterone enanthate or cypionate
- Transdermal patches or gels
- Implantable pellets or nasal formulations
TRT goals:
- Normalize serum testosterone
- Improve energy, sexual function, and lean muscle mass
- Prevent osteoporosis and maintain cardiovascular health
Fertility Considerations and Reproductive Counseling
- Semen cryopreservation should be offered when possible
- Assisted reproductive techniques (ART) may be necessary
- Endocrinologists should coordinate with fertility specialists for personalized care
Monitoring and Follow-Up
Routine follow-up includes:
- Serum testosterone, hematocrit, and lipid profiles
- Prostate health (PSA monitoring in older men)
- Bone density scans in patients with prolonged hypogonadism
- Mental health assessment due to increased risk of depression
Preventive Strategies
- Mumps vaccination (MMR) is essential to prevent viral orchitis
- Safe sexual practices reduce the risk of bacterial orchitis
- Early treatment of urinary tract infections and STIs
- Public health education targeting at-risk adolescent and young adult populations
Prognosis and Quality of Life
When promptly recognized and appropriately treated, the long-term health outcomes for men with primary hypogonadism due to orchitis can be favorable. However, irreversible infertility and lifelong hormonal dependence may occur. Multidisciplinary care and psychosocial support play a crucial role in holistic recovery.
Primary hypogonadism resulting from orchitis remains a significant yet underrecognized cause of male reproductive and hormonal dysfunction. Vigilant diagnostic efforts, prompt management of acute infection, and well-regulated hormonal therapy are imperative. Integrating endocrinology, urology, and mental health services ensures comprehensive patient-centered care.