Primary adrenocortical insufficiency, commonly known as Addison’s disease, is a rare yet critical endocrine disorder that affects the adrenal glands’ ability to produce essential hormones, including cortisol and aldosterone. These hormones are pivotal in regulating a variety of bodily functions, such as metabolism, immune response, and fluid balance. Without adequate hormone production, individuals with primary adrenocortical insufficiency may experience a range of symptoms that can severely impact their health. This article provides an in-depth exploration of primary adrenocortical insufficiency, its causes, symptoms, diagnosis, treatment options, and management strategies.
What is Primary Adrenocortical Insufficiency?
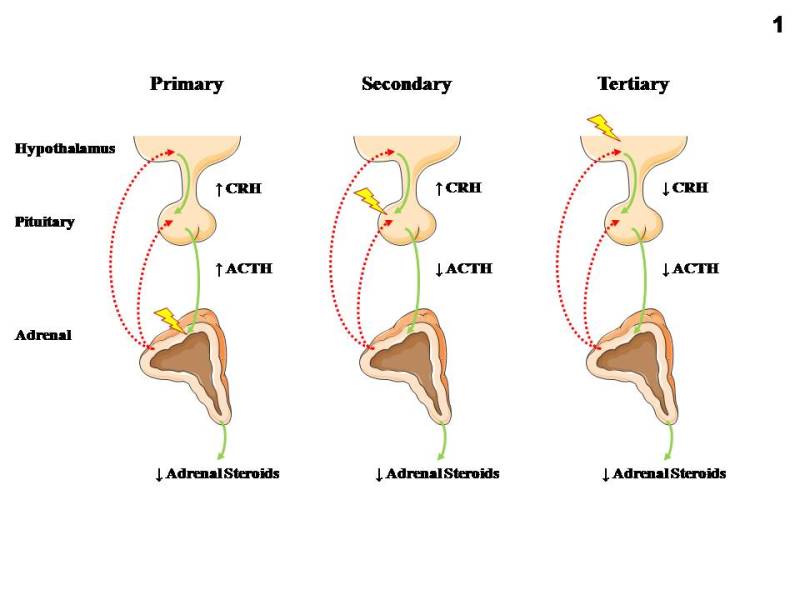
Primary adrenocortical insufficiency occurs when the adrenal glands, located above the kidneys, fail to produce sufficient amounts of cortisol and aldosterone. Cortisol plays a critical role in the body’s response to stress, metabolism, and immune function, while aldosterone helps regulate blood pressure and electrolyte balance. When the adrenal glands are damaged or impaired, the body cannot effectively maintain these functions, leading to a condition known as adrenal insufficiency.
The condition is most commonly referred to as Addison’s disease when it is caused by autoimmune destruction of the adrenal cortex. However, it can also result from infections, genetic disorders, or other underlying causes.
Causes of Primary Adrenocortical Insufficiency
The causes of primary adrenocortical insufficiency are varied, with autoimmune disease being the most common. However, other factors can also contribute to the development of this disorder.
Autoimmune Disease
- Autoimmune Addison’s Disease: In this condition, the immune system mistakenly attacks the adrenal cortex, impairing its ability to produce hormones. It is the leading cause of primary adrenocortical insufficiency in Western countries.
Infections
- Tuberculosis (TB): Tuberculosis can lead to the destruction of the adrenal glands, causing a condition known as Addison’s disease.
- Fungal Infections: In rare cases, fungal infections can also damage the adrenal glands, resulting in hormone deficiencies.
Genetic and Congenital Conditions
- Congenital Adrenal Hyperplasia (CAH): A genetic disorder that affects adrenal function and can lead to the development of primary adrenal insufficiency.
- Adrenoleukodystrophy (ALD): A rare genetic condition that can lead to adrenal gland dysfunction and subsequent insufficiency.
Cancer and Tumors
- Metastatic Cancer: Cancer from other parts of the body, such as lung or breast cancer, can spread to the adrenal glands and impair their function.
- Adrenal Gland Tumors: Tumors in the adrenal glands can also cause adrenal insufficiency, either by disrupting hormone production or through excessive hormone secretion.
Hemorrhage and Trauma
- Adrenal Hemorrhage: A condition where bleeding occurs in the adrenal glands, which can cause acute adrenal insufficiency. This is often seen in individuals with blood clotting disorders or after major trauma.
Symptoms of Primary Adrenocortical Insufficiency
The symptoms of primary adrenocortical insufficiency can vary significantly between individuals and often develop gradually. The most common symptoms are related to a deficiency in cortisol and aldosterone, which can affect a wide range of bodily functions.
Common Symptoms
- Fatigue and Weakness: A hallmark of Addison’s disease, individuals often feel constantly tired or weak, even after rest.
- Unexplained Weight Loss: Due to the body’s inability to effectively regulate metabolism.
- Low Blood Pressure (Hypotension): Cortisol helps regulate blood pressure, and its deficiency can result in persistent low blood pressure.
- Salt Cravings: Due to aldosterone deficiency, which leads to a reduction in sodium retention, individuals may experience intense cravings for salt.
- Hyperpigmentation: Darkening of the skin, particularly in areas exposed to the sun, as well as scars or skin folds, can occur due to an increase in melanocyte-stimulating hormone.
Other Symptoms
- Nausea and Vomiting: Often due to electrolyte imbalances or low cortisol levels.
- Abdominal Pain: Discomfort or cramping can be a common symptom, particularly in the early stages.
- Dizziness and Fainting: Low blood pressure and dehydration can cause individuals to feel lightheaded or faint, especially when standing up quickly.
Diagnosis of Primary Adrenocortical Insufficiency
Early diagnosis of primary adrenocortical insufficiency is essential to prevent complications such as adrenal crisis, a life-threatening condition that can occur when cortisol levels are critically low. Several diagnostic tests and procedures are used to confirm the presence of this disorder.
Blood Tests
- Cortisol Levels: A blood test measuring cortisol levels can help diagnose adrenal insufficiency. Low cortisol levels, especially in the morning, are indicative of the condition.
- ACTH Stimulation Test: In this test, the adrenocorticotropic hormone (ACTH) is administered, and the cortisol response is measured. In healthy individuals, cortisol levels should rise following ACTH stimulation, but in those with Addison’s disease, the response is often blunted or absent.
Imaging Studies
- CT Scan or MRI: These imaging studies can help identify any structural abnormalities in the adrenal glands, such as tumors or signs of adrenal atrophy.
Additional Tests
- Electrolyte Levels: Blood tests to measure sodium, potassium, and other electrolytes are essential for assessing aldosterone function, as deficiencies in this hormone can lead to electrolyte imbalances.
Treatment Options for Primary Adrenocortical Insufficiency
The treatment of primary adrenocortical insufficiency focuses on hormone replacement therapy to restore normal cortisol and aldosterone levels. Additionally, managing underlying conditions and preventing adrenal crises are critical components of treatment.
Hormone Replacement Therapy
- Cortisol Replacement: Synthetic glucocorticoids, such as hydrocortisone, prednisone, or dexamethasone, are used to replace cortisol. The dosage is individualized based on the patient’s needs and lifestyle.
- Aldosterone Replacement: Fludrocortisone is often prescribed to replace aldosterone, helping to regulate sodium and potassium levels and maintain blood pressure.
Acute Adrenal Crisis Management
An adrenal crisis is a life-threatening emergency that requires immediate medical attention. It can be triggered by stress, infection, injury, or insufficient medication. Treatment includes:
- Intravenous Hydrocortisone: To rapidly restore cortisol levels.
- Intravenous Fluids: To correct dehydration and electrolyte imbalances.
- Electrolyte Management: Correction of abnormal sodium and potassium levels is essential in managing adrenal crisis.
Ongoing Management
Once initial treatment is administered, individuals with primary adrenocortical insufficiency need ongoing hormone replacement therapy. Regular monitoring of hormone levels and clinical symptoms is crucial to adjust dosages as necessary.
Prevention and Long-Term Management
While primary adrenocortical insufficiency cannot be entirely prevented, individuals diagnosed with the condition can take several steps to minimize complications and manage their health effectively.
Stress Management
- Adrenal Crisis Prevention: Patients should be educated on how to adjust their hormone replacement doses during periods of physical stress, such as illness, surgery, or trauma. They may require higher doses of cortisol to manage stress.
Regular Monitoring
- Frequent Check-ups: Regular visits to an endocrinologist are essential to ensure that hormone levels remain balanced and that any complications are detected early.
- Electrolyte and Blood Pressure Monitoring: Continuous monitoring of electrolyte levels and blood pressure is important to avoid crises.
Primary adrenocortical insufficiency, or Addison’s disease, is a serious but manageable endocrine disorder. Early diagnosis, effective hormone replacement therapy, and ongoing medical management can significantly improve quality of life and prevent complications such as adrenal crisis. By understanding the causes, symptoms, and treatment options for primary adrenocortical insufficiency, individuals can take proactive steps to manage their condition and maintain optimal health. Regular follow-ups and stress management are crucial to ensuring long-term stability and preventing life-threatening episodes.