Vitamin D deficiency is a widespread global health issue, with implications that span from impaired bone mineralization to increased risks of chronic diseases. As a fat-soluble secosteroid, vitamin D plays a crucial role in calcium and phosphate homeostasis, immune modulation, and musculoskeletal integrity. We present a comprehensive strategy to prevent vitamin D deficiency, addressing its multifactorial causes and providing actionable interventions for individuals, healthcare providers, and policymakers.
The Vital Role of Vitamin D in Human Physiology
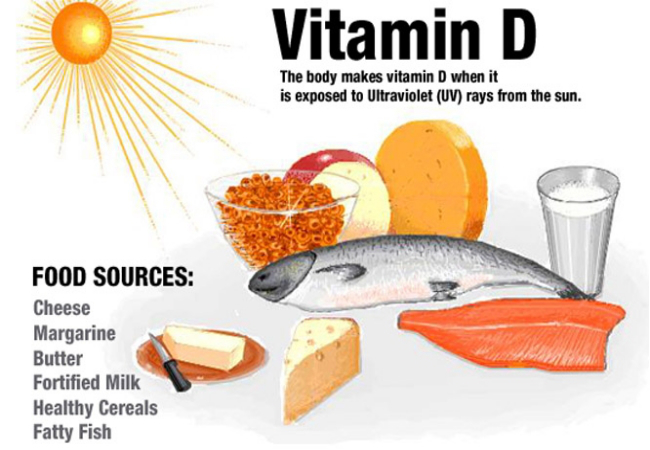
Vitamin D exists in two major forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Upon exposure to UVB radiation or dietary intake, vitamin D undergoes two hydroxylations in the liver and kidneys to form calcitriol (1,25-dihydroxyvitamin D), its active form.
Key physiological functions include:
- Calcium absorption in the gut and reabsorption in kidneys
- Bone remodeling and mineralization
- Immune system regulation, reducing inflammation
- Neuromuscular functioning and mood regulation
Identifying Risk Factors for Vitamin D Deficiency
Limited Sun Exposure
- Indoor lifestyles and urbanization reduce sun exposure
- Use of sunscreen and protective clothing
- Higher latitudes and winter seasons decrease UVB intensity
Skin Pigmentation
- Darker skin tones contain more melanin, which reduces vitamin D synthesis
Age and Physiology
- Elderly individuals have reduced skin capacity to produce vitamin D
- Obesity sequesters vitamin D in adipose tissue, limiting bioavailability
- Malabsorption syndromes such as celiac disease, Crohn’s disease, and cystic fibrosis
Chronic Health Conditions and Medications
- Liver or kidney disease impairs vitamin D metabolism
- Anticonvulsants, glucocorticoids, and antiretrovirals accelerate vitamin D breakdown
Early Signs and Symptoms of Vitamin D Deficiency
- Muscle weakness and proximal muscle pain
- Bone pain, rickets in children, and osteomalacia in adults
- Fatigue, low mood, and impaired immunity
- Increased risk of fractures, falls, and autoimmune conditions
Routine screening is advised in symptomatic individuals or those at high risk.
Optimizing Sunlight Exposure for Natural Vitamin D Synthesis
Recommended Guidelines
- 10–30 minutes of midday sun exposure on face, arms, and legs, several times per week
- UVB radiation is most effective between 10 a.m. and 3 p.m.
- Shorter exposure for lighter skin tones; longer for darker skin
Balancing Benefits and Skin Cancer Risk
- Encourage safe sun practices, avoiding sunburn while maximizing UVB exposure
- For regions with low sunlight, particularly during winter months, alternative strategies are critical
Nutritional Sources of Vitamin D: Food-Based Prevention
Naturally Rich Foods
- Fatty fish: Salmon, mackerel, sardines, and tuna
- Cod liver oil: Among the most concentrated sources
- Egg yolks, beef liver, and cheese
Fortified Foods
- Milk, breakfast cereals, orange juice, and plant-based milk alternatives
- Fortification is essential for vegan and vegetarian populations
Dietary Recommendations
| Age Group | Recommended Daily Allowance (RDA) |
|---|---|
| Infants (0–12 mo) | 400 IU (10 mcg) |
| Children & Adults | 600–800 IU (15–20 mcg) |
| Seniors (70+ yrs) | 800 IU (20 mcg) |
| Pregnant/Lactating | 600 IU (15 mcg) |
Supplementation Strategies: Ensuring Adequate Intake
Oral Supplements
- Vitamin D3 (cholecalciferol) is preferred due to superior efficacy
- Daily doses of 1,000–2,000 IU are safe for most adults
- Higher therapeutic doses (up to 50,000 IU weekly) may be used under medical supervision
Targeted Supplementation for At-Risk Populations
- Infants exclusively breastfed
- Elderly or homebound individuals
- People with malabsorption, obesity, or chronic illnesses
- Ethnic minorities with high melanin levels living in northern climates
Diagnostic and Monitoring Protocols
Laboratory Testing
- Serum 25-hydroxyvitamin D [25(OH)D] is the gold standard
- Deficiency: <20 ng/mL (50 nmol/L)
- Insufficiency: 20–30 ng/mL (50–75 nmol/L)
- Optimal: 30–60 ng/mL (75–150 nmol/L)
Monitoring Frequency
- At-risk individuals: biannual or annual testing
- General population: once every 2–3 years unless symptomatic
Public Health Interventions for Population-Wide Prevention
Fortification Policies
- National guidelines for mandatory vitamin D fortification
- Effective in reducing rickets and osteomalacia prevalence
Awareness Campaigns
- Promote sunlight exposure, dietary sources, and routine testing
- Public education in schools, community centers, and healthcare facilities
Health Professional Training
- Equip healthcare workers with skills to identify, prevent, and manage vitamin D deficiency
- Integrate screening into routine preventive care
Special Considerations in Vulnerable Groups
Pregnant and Lactating Women
- Adequate levels support fetal skeletal development
- Supplementation of 600–2,000 IU/day recommended
Infants and Children
- Vitamin D drops essential for exclusively breastfed infants
- Prevents rickets, supports growth and immunity
Elderly Population
- Combined vitamin D and calcium supplementation reduces fracture risk
- Prevents osteopenia, osteoporosis, and muscle atrophy
Preventing vitamin D deficiency requires a strategic integration of lifestyle, nutritional, and medical interventions tailored to both individual needs and broader public health initiatives. Through targeted sun exposure, a diet enriched with vitamin D, effective supplementation, and robust screening practices, we can safeguard bone integrity, immune resilience, and long-term wellness across populations. Sustained efforts in education, policy, and clinical care are essential to mitigate this silent yet impactful nutritional deficiency.