Stress ulcers are acute gastric mucosal lesions frequently encountered in critically ill patients, especially those in intensive care units (ICUs). These lesions can progress to stress-related mucosal disease (SRMD), often leading to upper gastrointestinal (GI) bleeding—a serious complication with high morbidity and mortality. Prophylactic strategies have been proven effective in reducing their incidence, necessitating a comprehensive understanding of the risk factors and evidence-based interventions.
Pathophysiology of Stress Ulcers and SRMD
Stress ulcers primarily arise from physiological stress that disrupts gastric mucosal integrity. The pathogenesis involves:
- Reduced mucosal blood flow
- Hypoperfusion-induced ischemia
- Increased acid secretion
- Decreased mucosal bicarbonate production
These changes compromise the mucosal barrier and lead to the development of superficial erosions or full-thickness ulcerations.
High-Risk Factors for Stress Ulcer Development
Effective prevention begins with identifying patients at elevated risk. The major risk factors include:
- Mechanical ventilation for >48 hours
- Coagulopathy (INR >1.5 or platelets <50,000/mm³)
- Severe burns (>35% total body surface area)
- Traumatic brain or spinal cord injury
- Sepsis and shock
- Prolonged ICU stay
- Use of high-dose corticosteroids or NSAIDs
Pharmacological Prophylaxis: Drug Classes and Protocols
Pharmacologic prophylaxis plays a central role in preventing stress ulcers in critically ill patients.
Proton Pump Inhibitors (PPIs)
PPIs, such as pantoprazole and esomeprazole, are preferred due to their potent acid suppression and favorable safety profile.
Advantages:
- Long duration of acid suppression
- Effective in reducing clinically significant bleeding
Considerations:
- Increased risk of ventilator-associated pneumonia (VAP) and Clostridioides difficile infection
Histamine-2 Receptor Antagonists (H2RAs)
Common agents include ranitidine and famotidine. Although slightly less effective than PPIs, they remain viable alternatives.
Advantages:
- Lower cost
- Fewer infectious complications compared to PPIs
Sucralfate
An aluminum hydroxide complex that forms a protective barrier over ulcers.
Advantages:
- Does not alter gastric pH
- Minimal systemic absorption
Limitations:
- Less effective in preventing bleeding than PPIs or H2RAs
- Potential for aluminum toxicity in renal impairment
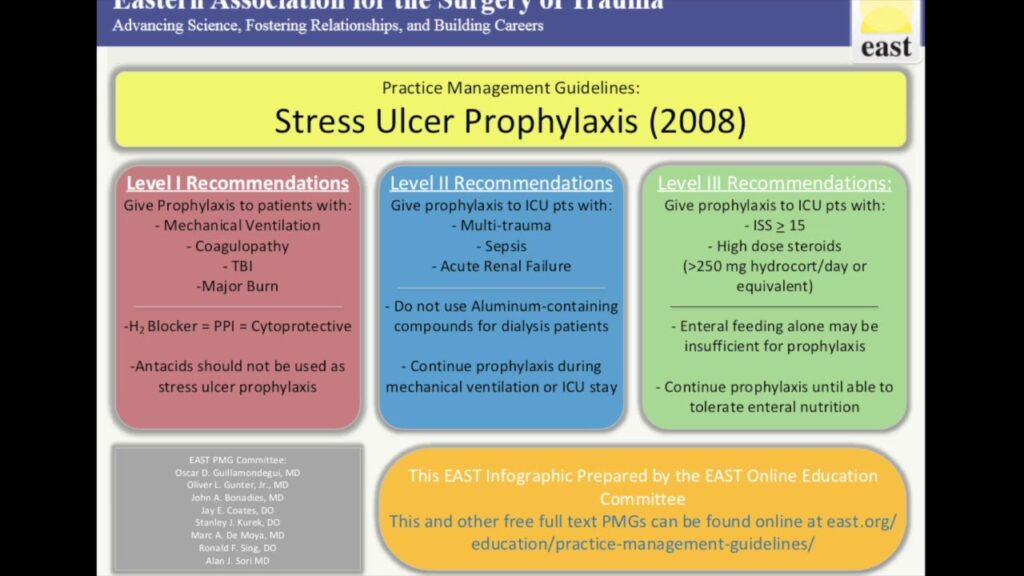
Indications for Stress Ulcer Prophylaxis (SUP)
SUP is not universally indicated for all ICU patients. Guidelines recommend its use in:
- Patients with major risk factors
- Patients with ≥2 minor risk factors (e.g., ICU stay >7 days, occult GI bleeding >6 days, corticosteroid therapy)
SUP should be reevaluated regularly and discontinued when risk factors resolve to prevent overtreatment.
Non-Pharmacological Approaches
Early Enteral Nutrition
Initiating enteral feeding within 24–48 hours of ICU admission promotes mucosal integrity and reduces stress ulcer risk.
Benefits:
- Enhances mucosal blood flow
- Stimulates bicarbonate secretion
- Maintains gastric motility
Avoidance of Unnecessary Medications
Restricting NSAIDs and corticosteroids can significantly reduce mucosal injury risk. When unavoidable, co-administration of protective agents is recommended.
Stress Ulcer Prevention in Specific Populations
Pediatric Intensive Care
Children in ICUs also face SRMD risks, though the incidence is lower. Tailored protocols should consider age-specific pharmacokinetics and risk stratification.
Postoperative and Surgical Patients
Patients undergoing major surgery, particularly cardiac or abdominal, benefit from perioperative prophylaxis if risk factors are present.
Monitoring and Discontinuation Guidelines
Excessive use of SUP increases the risk of adverse effects. Therefore, we recommend the following discontinuation criteria:
- Absence of mechanical ventilation or coagulopathy
- Initiation of oral/enteral feeding
- Transfer out of ICU or resolution of primary illness
Evidence-Based Prevention for Optimal Outcomes
Stress ulcer prevention is a critical aspect of ICU care. Through early identification of risk factors, judicious use of pharmacologic agents, and incorporation of enteral nutrition, healthcare teams can significantly reduce the incidence of SRMD and improve patient outcomes. Rational, evidence-driven prophylaxis not only safeguards patients but also minimizes unnecessary drug exposure and its associated risks.

