Skeletal-related events (SREs) in multiple myeloma (MM) represent a major cause of morbidity and impaired quality of life. These events, including pathologic fractures, spinal cord compression, need for radiation or surgery to bone, and hypercalcemia, arise from osteolytic bone lesions caused by myeloma-induced bone destruction.
Our goal in managing MM is not only to control the malignancy but also to prevent SREs through prophylactic, therapeutic, and supportive strategies that preserve skeletal integrity and reduce complications.
Pathophysiology of Bone Disease in Multiple Myeloma
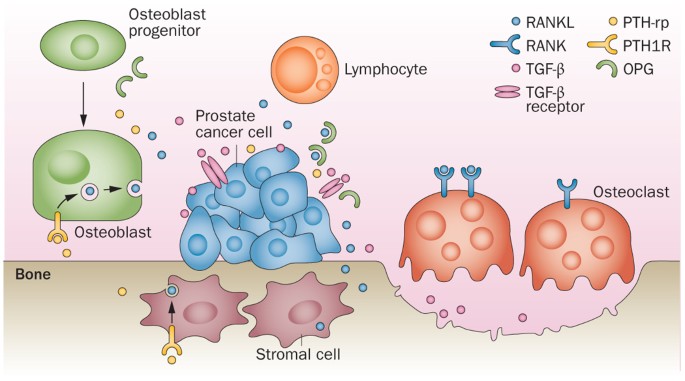
Myeloma bone disease results from an imbalance between osteoclastic bone resorption and suppressed osteoblastic activity, driven by the interaction between malignant plasma cells and the bone marrow microenvironment.
Key mechanisms include:
- RANK/RANKL pathway activation → Promotes osteoclastogenesis
- Suppression of osteoprotegerin (OPG) → Removes inhibition of bone resorption
- Cytokines like IL-6, MIP-1α → Enhance osteoclast survival
- Inhibition of Wnt signaling → Blocks osteoblast differentiation
The result is rapid bone degradation, which underlies the majority of SREs in MM patients.
Risk Factors for Skeletal-Related Events in MM
Understanding patient-specific and disease-related risk factors helps guide SRE prevention:
- Extensive lytic lesions at diagnosis
- High tumor burden
- Elevated serum calcium levels
- Advanced age or frailty
- Pre-existing osteoporosis or prior fractures
- Low bone mineral density (BMD)
- Immobility or steroid use
Routine imaging (PET-CT, MRI, low-dose whole-body CT) and biochemical markers are critical for early detection and monitoring.
Antiresorptive Therapy in the Prevention of SREs
1. Bisphosphonates: First-Line Anti-Bone Resorption Agents
Zoledronic acid and pamidronate are key agents for preventing SREs by inhibiting osteoclast-mediated bone destruction.
Zoledronic Acid
- Dose: 4 mg IV every 4 weeks
- Effectiveness: Reduces fracture risk, delays SREs, improves survival in some patients
- Caution: Renal toxicity—monitor creatinine levels; consider dose adjustments
Pamidronate
- Dose: 90 mg IV over 2 hours every 4 weeks
- Alternative: For patients intolerant to zoledronic acid
Bisphosphonates are continued for up to 2 years, with reevaluation for patients in sustained remission.
2. Denosumab: An Alternative in Renal Impairment
Denosumab is a fully human monoclonal antibody targeting RANKL, preventing osteoclast formation and function.
- Dose: 120 mg subcutaneously every 4 weeks
- Advantages: No renal clearance; ideal for patients with renal insufficiency
- Monitoring: Serum calcium, vitamin D, and magnesium levels
Clinical Evidence:
- Phase 3 trials showed non-inferiority to zoledronic acid in delaying SREs, with favorable renal safety profile.
Adjunctive Measures for Bone Health Preservation
Calcium and Vitamin D Supplementation
- Calcium: 1,000–1,200 mg daily
- Vitamin D3: 800–1,000 IU daily
- Required to reduce hypocalcemia risk, especially with denosumab use.
Weight-Bearing Exercise
- Helps maintain bone strength, prevent falls, and enhance mobility
- Tailored to patient capability and fracture risk
Pain Management
- SREs often result in severe bone pain
- Treatment includes analgesics, bisphosphonates, radiotherapy, and surgical stabilization
Orthopedic and Radiotherapy Interventions
- Vertebroplasty/kyphoplasty for spinal compression
- Surgical fixation for long bone fractures
- Palliative radiotherapy for pain control and local disease management
Monitoring and Duration of Antiresorptive Therapy
Evaluation Timeline:
| Parameter | Frequency |
|---|---|
| Serum creatinine | Before each dose |
| Calcium and Vitamin D | Monthly or as needed |
| Bone imaging | Every 6–12 months |
| Dental examination | Prior to therapy initiation |
Osteonecrosis of the jaw (ONJ) is a rare but serious adverse effect; maintain excellent oral hygiene and avoid invasive dental procedures during therapy.
Therapy Duration Recommendations:
- Standard treatment: 12–24 months
- Maintenance phase: Extend dosing interval or pause in deep remission
- Restart therapy: Upon biochemical or radiographic relapse
Integration with Systemic Anti-Myeloma Therapy
Proteasome inhibitors, immunomodulators, and monoclonal antibodies help reduce bone turnover indirectly by:
- Lowering tumor burden
- Suppressing pro-osteoclast cytokines
- Promoting partial osteoblast activity recovery
Combining antiresorptive therapy with systemic agents ensures a multimodal approach to SRE prevention.
Future Directions in SRE Management
Emerging Therapies:
- Cathepsin K inhibitors: Inhibit osteoclast function with bone-forming potential
- Sclerostin inhibitors (e.g., romosozumab): Promote osteoblast activity
- Bi-specific antibodies and CAR-T therapy: Reduce marrow tumor cells more effectively
These novel approaches may reshape how bone health is maintained in MM patients.
Summary of Key Recommendations
- Initiate antiresorptive therapy (bisphosphonates or denosumab) in MM patients with lytic bone lesions
- Use denosumab in patients with renal impairment
- Supplement with calcium and vitamin D
- Monitor renal function, serum calcium, and dental health throughout treatment
- Reevaluate therapy duration based on disease status and toxicity
- Integrate supportive care and physical rehabilitation to reduce SRE risk
Frequently Asked Questions
What are skeletal-related events in multiple myeloma?
SREs include fractures, spinal cord compression, need for radiation or surgery to bone, and hypercalcemia due to bone destruction in MM.
Which drug is best for SRE prevention in MM patients with kidney problems?
Denosumab is preferred due to its safety profile in patients with renal impairment.
Can SREs be completely prevented in MM?
While not always preventable, their incidence and severity can be significantly reduced with proper therapy and monitoring.
How long should bisphosphonates be continued?
Typically 12 to 24 months, with adjustments based on disease status and response.
Are there side effects with antiresorptive therapies?
Yes. Possible effects include renal dysfunction, hypocalcemia, and osteonecrosis of the jaw, requiring close monitoring.

