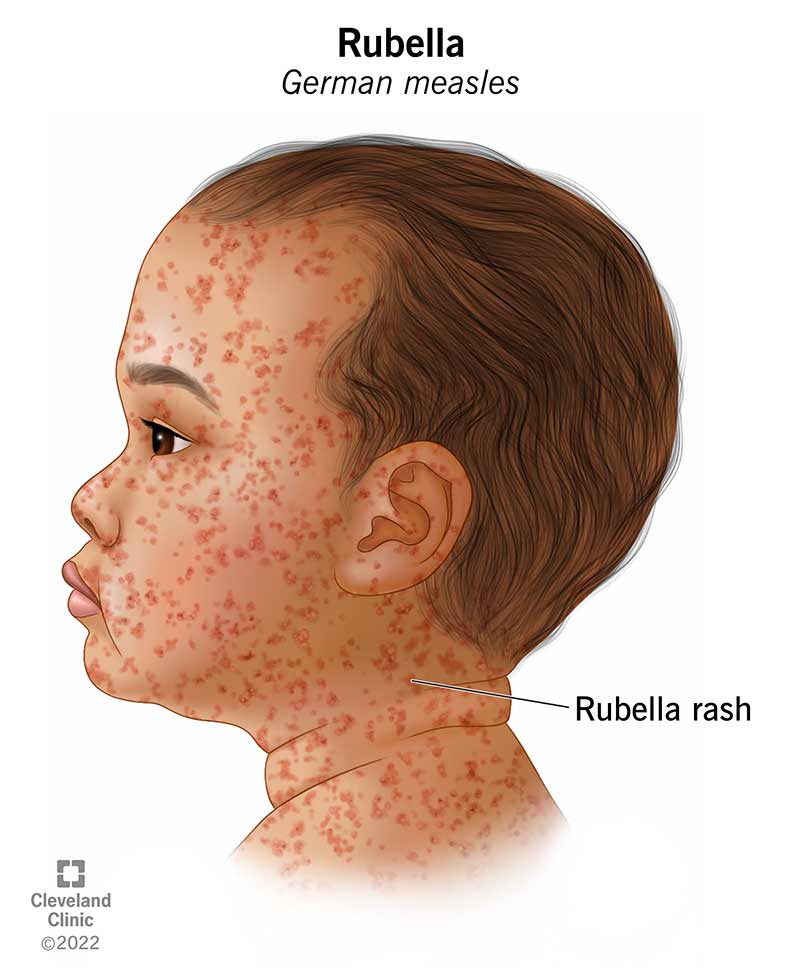
Rubella, also known as German measles, is a contagious viral infection caused by the rubella virus, primarily transmitted via respiratory droplets. Although typically mild in children and adults, rubella poses a significant threat during pregnancy, particularly in the first trimester, due to its association with congenital rubella syndrome (CRS). CRS can lead to serious fetal anomalies including deafness, cataracts, cardiac defects, and intellectual disabilities.
Efficient prevention of rubella following exposure is essential to protect vulnerable populations and limit outbreaks, especially in healthcare and community settings.
Modes of Rubella Transmission and Exposure Scenarios
Rubella is spread person-to-person through:
- Airborne droplets from coughs or sneezes
- Direct contact with infected nasal or throat secretions
- Congregate settings, including schools, clinics, or childcare facilities
High-risk exposure includes prolonged close contact with an infected individual during their infectious period, which typically ranges from 7 days before to 7 days after rash onset.
Post-Exposure Prophylaxis: First-Line Preventive Strategies
1. MMR Vaccination Post-Exposure
The measles-mumps-rubella (MMR) vaccine is not effective as post-exposure prophylaxis against rubella if administered after exposure has occurred. However, it plays a critical role in future immunity and outbreak containment.
- Recommendation: Individuals not previously vaccinated should receive the MMR vaccine immediately, especially during outbreak settings.
- Note: The vaccine is contraindicated in pregnant women and those with severe immunodeficiency.
2. Use of Rubella-Specific Immune Globulin (IG)
Immune globulin (IG) may be considered in select cases, particularly:
- Pregnant women without documented rubella immunity who have been exposed
- Infants under 6 months in rare circumstances
While IG does not guarantee prevention, it may attenuate infection. The recommended dose is 20 mL of intramuscular IG within 72 hours of exposure.
Rubella Immunity Testing and Serologic Screening
Post-exposure, rubella IgG antibody titers should be evaluated to determine immunity status:
- Immune: IgG positive; no further action required
- Non-immune: IgG negative; evaluate based on risk category
- Recent infection or seroconversion: IgM positive; initiate contact tracing and isolate accordingly
This step is critical in pregnancy, where outcomes are directly affected by maternal immunity.
Rubella in Pregnancy: Prevention and Management Post-Exposure
1. Risk to the Fetus
Infections occurring within the first 12 weeks of gestation pose up to a 90% risk of CRS. The risk declines with advancing gestation.
2. Management Steps for Pregnant Women
- Serologic testing for rubella IgG and IgM
- If IgG negative and IgM negative, consider:
- Expectant management with close monitoring
- Counseling on CRS risks
- Possible administration of immune globulin (20 mL IM) if requested, understanding it does not eliminate risk
- If IgM positive, initiate ultrasound surveillance, amniocentesis for rubella PCR, and refer for perinatology consultation
3. Pregnancy Termination Considerations
In confirmed fetal infection with severe anomalies, termination may be discussed, depending on gestational age, local laws, and parental preferences.
Healthcare Worker and Community Exposure Response
In institutional settings such as hospitals or schools:
- Assess immunity status of all exposed individuals
- Exclude susceptible individuals from duty or school for 21 days after last exposure
- Provide MMR vaccination to non-immune persons where appropriate
Healthcare workers, in particular, must have documented rubella immunity to prevent nosocomial outbreaks and protect pregnant patients.
Isolation and Infection Control Measures
- Isolation of rubella cases is required for 7 days after rash onset
- Infected individuals should avoid contact with pregnant women
- Implement droplet precautions in clinical settings
- Emphasize hand hygiene, mask use, and ventilation in outbreak control
Surveillance and Public Health Notification
All confirmed rubella cases must be reported to public health authorities to facilitate:
- Contact tracing
- Cluster investigation
- Vaccination outreach
- Epidemiological monitoring
This is essential to prevent large-scale outbreaks and uphold elimination goals in regions where rubella is no longer endemic.
Role of Preconception Vaccination in Long-Term Rubella Control
The most effective strategy for rubella prevention is routine MMR vaccination, ideally prior to pregnancy. Women of childbearing age should have documented immunity or receive MMR vaccine at least one month before conception.
Routine two-dose schedules provide lifelong immunity in most individuals, forming the foundation of rubella elimination programs worldwide.
Prevention of rubella after exposure requires a structured, risk-based approach that prioritizes immunity verification, appropriate prophylaxis, and public health collaboration. While no post-exposure intervention guarantees complete protection, early identification, vaccination of non-pregnant individuals, and administration of immune globulin in select cases significantly reduce transmission risk. Emphasizing preconception vaccination and immunity screening remains the most reliable method to eliminate rubella and prevent congenital rubella syndrome.