Rh isoimmunization, or Rh alloimmunization, is a potentially serious immunologic reaction that occurs when an Rh-negative individual is exposed to Rh-positive red blood cells (RBCs), typically via blood transfusion. This exposure prompts the immune system to develop anti-D antibodies, leading to complications such as hemolytic transfusion reactions and future incompatibility in transfusion or pregnancy scenarios.
Preventing Rh isoimmunization after blood transfusion is critical, especially in women of childbearing age and individuals requiring repeated transfusions. Effective preventive protocols protect against sensitization and maintain transfusion safety standards.
Mechanism of Rh Isoimmunization After Transfusion
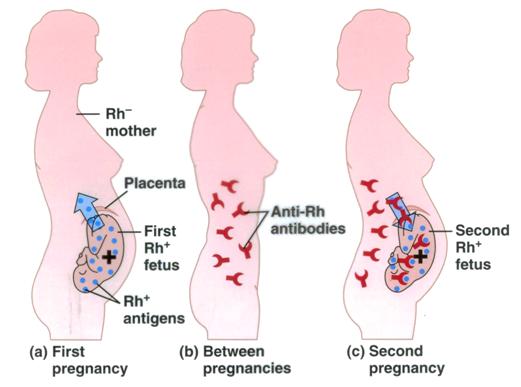
When Rh(D)-positive red blood cells are transfused into an Rh(D)-negative recipient, the immune system may recognize the D antigen as foreign. This recognition triggers:
- Primary immune response (first exposure): IgM antibodies are produced, which do not cross the placenta.
- Secondary immune response (subsequent exposures): IgG anti-D antibodies are produced, which can cross the placenta or mediate hemolysis in transfusions.
This sensitization process can be irreversible and dangerous.
Identifying At-Risk Patients for Rh Sensitization
The following patient populations require special consideration:
- Rh-negative individuals, especially females of reproductive age
- Patients with chronic transfusion needs, such as those with sickle cell anemia or thalassemia
- Patients undergoing organ transplants or major surgeries
- Neonates and pediatric patients requiring exchange transfusions
Proper screening and typing are mandatory before any transfusion.
Blood Typing and Antibody Screening Protocol
Pre-Transfusion Testing
To prevent Rh isoimmunization, pre-transfusion procedures must include:
- ABO and RhD typing of both donor and recipient
- Indirect Coombs test (antibody screen) to detect existing alloantibodies
- Crossmatch testing to ensure donor RBCs are serologically compatible
All testing must be completed before transfusion to avoid immunologic complications.
Preventive Measures and Strategies
Selection of Rh-Compatible Blood
- Rh-negative individuals must receive Rh-negative RBCs, particularly females of childbearing potential.
- In emergency situations where Rh-negative units are unavailable, Rh-positive units may be given with concurrent prophylaxis, under strict clinical judgment.
Use of Anti-D Immunoglobulin (RhIg)
Administering anti-D immunoglobulin is an effective preventive measure in non-alloimmunized Rh-negative recipients exposed to Rh-positive RBCs.
Indications
- Inadvertent transfusion of Rh-positive blood to an Rh-negative recipient
- Exchange transfusions in Rh-negative neonates
- Rh-incompatible platelet transfusions containing residual RBCs
Dosage and Administration
- Standard dose: 300 µg intramuscularly
- Protects against exposure to up to 15 mL of Rh-positive RBCs
- Must be administered within 72 hours of exposure to prevent sensitization
Monitoring and Post-Transfusion Management
Follow-Up Testing
After suspected Rh-incompatible transfusion:
- Repeat indirect Coombs test at 4–6 weeks
- Monitor for delayed hemolytic transfusion reactions
- Document antibody development for future transfusion planning
Special Considerations in Massive Transfusions
In trauma or massive transfusion protocols, Rh-negative patients, particularly females of reproductive age, must be prioritized for Rh-negative blood. If Rh-positive blood is used:
- Post-exposure RhIg administration is mandatory
- Use leukoreduced and irradiated components when appropriate to minimize immunologic complications
Blood Bank and Hospital Policy Recommendations
To institutionalize Rh isoimmunization prevention:
- Mandatory RhD typing on all recipients before transfusion
- Electronic flags in patient records for Rh-negative individuals
- Standard operating procedures for administration of RhIg in accidental exposures
- Blood inventory management to ensure adequate Rh-negative supply
Prevention of Rh isoimmunization after blood transfusion is a critical component of transfusion safety and long-term patient care. By ensuring Rh compatibility, administering anti-D immunoglobulin when necessary, and closely monitoring sensitization risk, healthcare providers can prevent severe immunologic reactions and maintain transfusion efficacy. Meticulous adherence to protocols and proactive blood bank practices remain the cornerstone of this preventive strategy.

