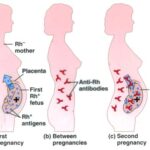
Rh incompatibility occurs when an Rh-negative mother carries an Rh-positive fetus, leading to the maternal immune system recognizing fetal red blood cells as foreign and producing antibodies. This sensitization can result in hemolytic disease of the fetus and newborn (HDFN), a serious condition that may cause anemia, jaundice, or even fetal death if not managed appropriately.
The Importance of Preventing Rh Sensitization
Preventing Rh sensitization is paramount to protecting the health of both the fetus and future pregnancies. Once sensitization has occurred, it cannot be reversed, and subsequent pregnancies are at high risk for HDFN. Therefore, timely and appropriate prophylactic measures are essential.
Risk Factors for Rh Incompatibility
- Rh-negative maternal blood type
- Rh-positive paternal or fetal blood type
- Invasive prenatal procedures (amniocentesis, chorionic villus sampling)
- Abdominal trauma during pregnancy
- Miscarriage or ectopic pregnancy
- Bleeding during pregnancy
- Delivery of an Rh-positive infant
Screening and Diagnosis of Rh Incompatibility
Maternal Blood Typing and Antibody Screening
All pregnant women should undergo blood typing and an indirect Coombs test early in pregnancy:
- Blood Typing: Determines ABO and Rh(D) status.
- Indirect Coombs Test: Detects the presence of anti-D antibodies in maternal serum.
Paternal and Fetal Rh Status
If the mother is Rh-negative, determining the Rh status of the father can help assess risk. Non-invasive prenatal testing (NIPT) can detect fetal Rh status using cell-free fetal DNA from maternal blood.
Prevention of Rh Incompatibility Reaction: Clinical Protocols
Administration of Anti-D Immunoglobulin (RhIg)
Anti-D immunoglobulin is the cornerstone of Rh incompatibility prevention. It works by neutralizing Rh-positive fetal red blood cells in the maternal circulation before the immune system can mount a response.
Prophylactic Administration Timeline
| Timing | Indication |
|---|---|
| 28 Weeks Gestation | Routine antenatal prophylaxis for all unsensitized Rh-negative women |
| Within 72 Hours Postpartum | If the newborn is Rh-positive |
| Following Risk Events | Miscarriage, abortion, ectopic pregnancy, trauma, bleeding, or invasive procedures |
Dosage
- Standard dose: 300 µg intramuscularly
- Provides protection against approximately 15 mL of fetal red blood cells
Efficacy
When administered appropriately, RhIg can prevent sensitization in over 99% of at-risk pregnancies.
Monitoring for Sensitization
Even with prophylaxis, continuous monitoring through repeat antibody screening at 28 weeks and postpartum is necessary to ensure no sensitization has occurred.
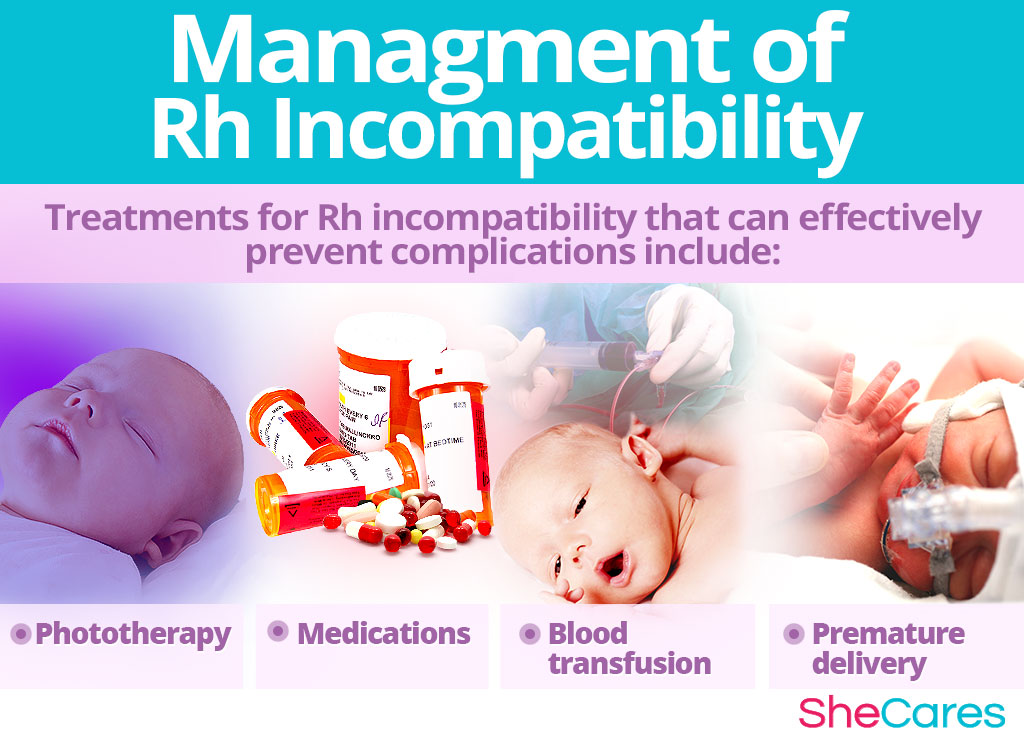
Management of Sensitized Pregnancies
If sensitization occurs, pregnancies require specialized care:
- Serial Antibody Titer Monitoring
- Middle Cerebral Artery (MCA) Doppler Ultrasound to detect fetal anemia
- Intrauterine Transfusion (IUT) in severe cases of fetal anemia
- Early Delivery if fetal distress is detected
Future Pregnancies and Preconception Counseling
Women with prior sensitization or a history of Rh incompatibility should receive:
- Genetic counseling and pre-pregnancy planning
- Early prenatal care and screening
- High-risk obstetric consultation
Role of Public Health and Education
Public health initiatives and healthcare provider education play a vital role in the prevention of Rh disease by:
- Ensuring universal access to Rh typing and RhIg
- Educating patients on the importance of follow-up care
- Promoting adherence to prophylaxis guidelines
The prevention of Rh incompatibility reaction is a critical component of modern obstetric care. Through early identification of at-risk pregnancies, timely administration of anti-D immunoglobulin, and vigilant monitoring, we can drastically reduce the incidence of Rh sensitization and hemolytic disease of the fetus and newborn. Comprehensive prenatal care and public awareness remain key pillars in safeguarding maternal and neonatal health.