Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, characterized by rapid, irregular atrial activity. Recurrent atrial fibrillation refers to the return of arrhythmic episodes after initial restoration of normal sinus rhythm, either spontaneously or through therapeutic intervention. Recurrence rates are significant—up to 70% within the first year in untreated cases—underscoring the need for robust prevention strategies.
Pathophysiology and Triggers of AF Recurrence
AF recurrence is driven by a complex interplay between electrical remodeling, structural fibrosis, and systemic triggers. Common initiating and perpetuating factors include:
- Left atrial enlargement
- Hypertension and heart failure
- Sleep apnea
- Thyroid dysfunction
- Alcohol intake
- Inflammation and oxidative stress
- Obesity and metabolic syndrome
These elements promote reentry circuits and ectopic foci, primarily within the pulmonary veins, contributing to AF recurrence.
Diagnostic Framework for Recurrence Risk Assessment
To tailor effective preventive measures, risk stratification is essential. The following tools and parameters are used:
| Parameter | Clinical Relevance |
|---|---|
| CHA₂DS₂-VASc Score | Stroke risk prediction |
| Left atrial volume/index | Structural substrate of AF |
| NT-proBNP | Marker of atrial stretch/failure |
| 24–48h Holter/implantable loop | AF burden and recurrence monitoring |
| Sleep study (polysomnography) | Identifies obstructive sleep apnea |
Medical Therapy for Rhythm and Rate Control
Antiarrhythmic Drug Therapy
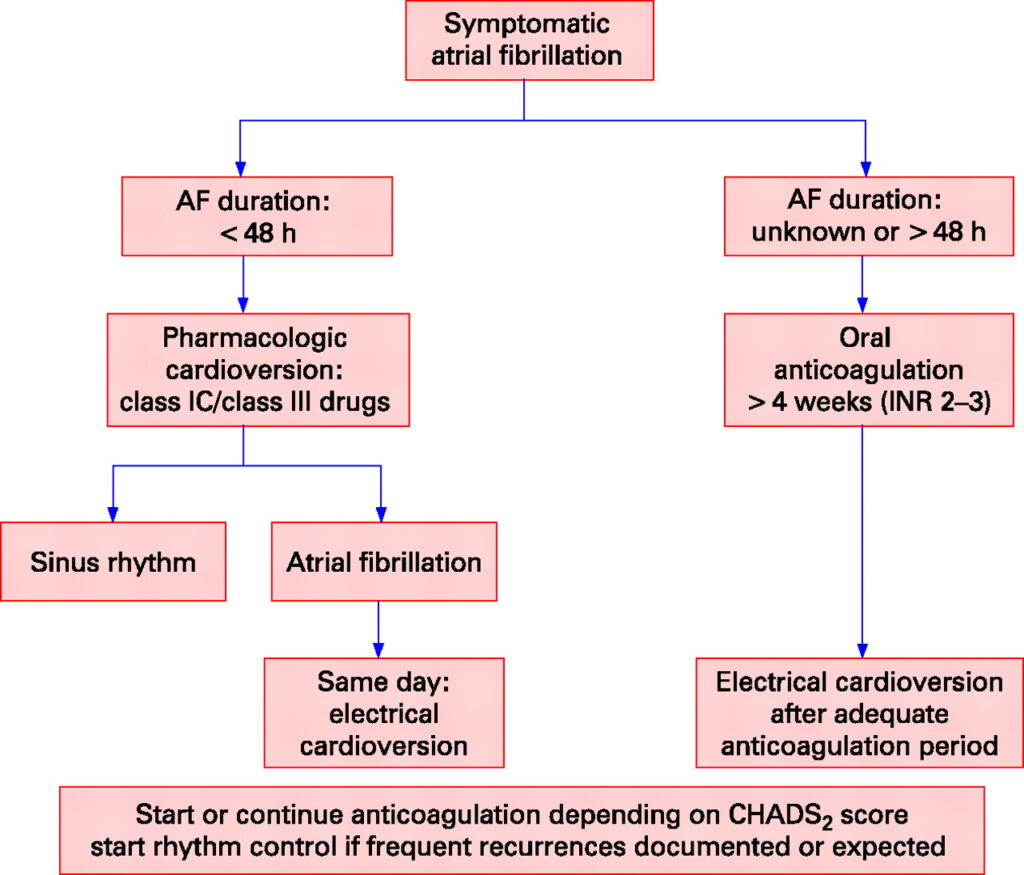
Rhythm control remains a core strategy, particularly for symptomatic or high-risk patients. First-line agents include:
| Drug | Class | Indication |
|---|---|---|
| Flecainide | IC | Paroxysmal AF, structurally normal hearts |
| Propafenone | IC | Mild structural heart disease |
| Dronedarone | III | Reduced recurrence in non-permanent AF |
| Sotalol | III | Effective but with proarrhythmic potential |
| Amiodarone | III | Most effective, used in heart failure/structural heart disease |
Regular QT monitoring and renal function assessment are vital in patients on Class III drugs.
Rate Control as an Adjunct
If rhythm control fails or is contraindicated, rate control is crucial:
- Beta-blockers (e.g., metoprolol)
- Non-dihydropyridine calcium channel blockers (verapamil, diltiazem)
- Digoxin (in sedentary individuals or heart failure patients)
Catheter Ablation: A Definitive Strategy for Refractory Cases
Pulmonary vein isolation (PVI) via radiofrequency or cryoballoon ablation offers superior freedom from recurrence compared to medical therapy in select populations.
Indications for Ablation:
- Symptomatic paroxysmal or persistent AF refractory to drug therapy
- Patient preference for rhythm control
- Heart failure with reduced ejection fraction (HFrEF) where AF exacerbates symptoms
Recurrence Post-Ablation
Approximately 20–30% experience recurrence within 1 year due to:
- Incomplete isolation
- Atrial scarring
- Triggering foci outside pulmonary veins
Repeat ablation and adjunctive lesion sets may be warranted in such cases.
Comprehensive Lifestyle Modification: A Cornerstone of Long-Term AF Control
1. Weight Reduction and Metabolic Optimization
Obesity is a potent and modifiable AF risk factor. A ≥10% weight loss significantly reduces recurrence rates.
- Target BMI: 18.5–24.9 kg/m²
- Structured weight management programs
- Management of diabetes and dyslipidemia
2. Treatment of Sleep Apnea
Obstructive sleep apnea is highly prevalent in AF patients. Continuous positive airway pressure (CPAP) therapy reduces both AF burden and recurrence post-ablation.
3. Alcohol and Caffeine Moderation
- Avoid binge drinking (“holiday heart syndrome”)
- Limit alcohol to <2 standard drinks/day for men, <1 for women
- Moderate caffeine intake is generally safe
4. Physical Activity
Moderate aerobic exercise (≥150 minutes/week) improves cardiovascular fitness and lowers AF recurrence risk. Excessive endurance training, however, may promote AF.
Anticoagulation Considerations in AF Recurrence
Even in rhythm-controlled patients, the stroke risk persists. Anticoagulation is guided by the CHA₂DS₂-VASc score, independent of sinus rhythm maintenance.
- NOACs (Apixaban, Rivaroxaban, Dabigatran) are preferred over warfarin due to favorable safety profiles.
- Lifelong anticoagulation may be warranted in high-risk individuals despite ablation success.
Role of Anti-inflammatory and Upstream Therapies
Emerging evidence supports the role of systemic inflammation in AF pathogenesis. Novel preventive measures include:
- Statins: Especially beneficial in postoperative AF and patients with elevated CRP
- Omega-3 fatty acids: May reduce AF episodes via anti-inflammatory effects
- RAAS inhibitors (ACEi/ARB): Beneficial in patients with hypertension or LV dysfunction
Post-Treatment Surveillance and Follow-Up
A structured follow-up regimen is essential to detect asymptomatic recurrences, adjust therapy, and reinforce lifestyle changes:
| Timeline | Actions |
|---|---|
| 1–3 months | ECG, symptom review, adjust medications |
| 6 months | Holter monitoring or implantable loop recorder |
| Annually | Risk reassessment, echo if structural changes suspected |
Preventing recurrent atrial fibrillation requires a tailored, evidence-based strategy combining pharmacologic intervention, lifestyle transformation, procedural solutions, and ongoing surveillance. Weight management, sleep apnea treatment, and targeted rhythm control—especially through ablation in selected patients—offer a multifaceted approach that significantly improves long-term outcomes and quality of life. By integrating these components, we enhance our ability to maintain sinus rhythm and reduce AF-related morbidity.