Radiation therapy-induced mucositis is a common and debilitating complication in patients undergoing radiotherapy for head and neck cancers. Characterized by erythema, ulceration, and pain of the oral mucosa, mucositis adversely affects nutritional intake, oral hygiene, treatment compliance, and overall quality of life. Preventing mucositis is imperative to maintaining uninterrupted cancer treatment and reducing morbidity.
Pathophysiology of Oral Mucositis in Radiotherapy
Mucositis follows a five-phase biological process:
- Initiation: Direct DNA damage and reactive oxygen species (ROS) formation
- Upregulation: Release of pro-inflammatory cytokines (e.g., TNF-α, IL-1β)
- Signal amplification: Cascading tissue injury
- Ulceration: Bacterial colonization and severe mucosal damage
- Healing: Cellular proliferation and re-epithelialization
Radiation exacerbates this cycle by targeting rapidly dividing basal epithelial cells, compromising mucosal integrity and promoting ulceration.
Risk Factors Enhancing Mucositis Susceptibility
- High radiation dose (>60 Gy)
- Concomitant chemotherapy (e.g., cisplatin)
- Poor oral hygiene
- Pre-existing dental disease
- Smoking and alcohol use
- Nutritional deficiencies
Evidence-Based Preventive Strategies
1. Optimal Oral Hygiene Protocols
Maintaining meticulous oral hygiene reduces bacterial load and minimizes mucosal irritation.
Clinical Recommendations:
- Brush with a soft-bristled toothbrush after meals
- Use non-alcoholic fluoride mouth rinses
- Perform saline or sodium bicarbonate rinses 4–6 times daily
2. Low-Level Laser Therapy (LLLT)
LLLT stimulates epithelial regeneration, reduces inflammation, and alleviates pain.
Protocol:
- Wavelength: 632–660 nm
- Dose: 2–4 J/cm² per application site
- Frequency: 3–5 sessions per week throughout radiotherapy
3. Cryotherapy
Cryotherapy is particularly effective in chemotherapy-induced mucositis and has emerging support for radiation-related cases.
Mechanism:
Cold-induced vasoconstriction minimizes drug delivery and tissue damage in mucosa.
Application:
- Ice chips held in the mouth for 30 minutes during radiation/chemo infusion
4. Topical Mucosal Protectants
Barrier-forming agents create a protective film over the mucosa, reducing friction and microbial infiltration.
Examples:
- Sucralfate suspension
- Gelclair®
- Caphosol®
These agents coat ulcerated areas and reduce pain perception.
5. Use of Amifostine
Amifostine is a cytoprotective agent shown to reduce the incidence and severity of mucositis.
Dosage:
- 200–300 mg/m² administered intravenously 15–30 minutes before radiation
Limitations:
- Side effects include hypotension and nausea
- Reserved for high-risk or refractory cases
6. Palifermin (Recombinant Human Keratinocyte Growth Factor)
Palifermin stimulates epithelial cell proliferation and is FDA-approved for preventing mucositis in patients receiving high-dose chemotherapy and radiotherapy prior to stem cell transplant.
Dose and Use:
- 60 μg/kg/day IV for 3 days before and after treatment
Consideration:
- Limited to select patients due to cost and specific indications
Nutritional and Supportive Interventions
Adequate nutrition is crucial to tissue repair and immune function. Implement:
- High-protein, soft diets
- Oral nutritional supplements
- Hydration support
- Avoidance of acidic, spicy, and rough foods
When oral intake becomes inadequate:
- Initiate enteral nutrition via nasogastric or PEG tube
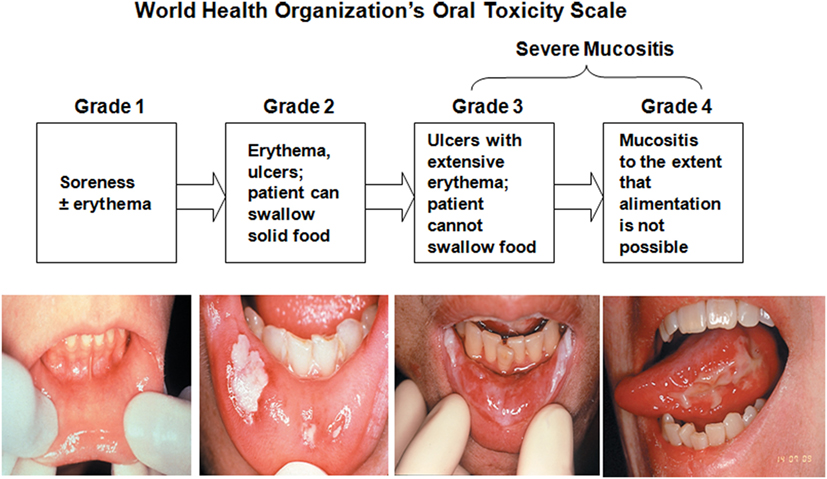
Clinical Monitoring and Grading of Mucositis
Standardized assessment ensures early intervention and treatment adjustment.
WHO Mucositis Grading Scale:
| Grade | Description |
|---|---|
| 0 | No symptoms |
| 1 | Erythema and soreness |
| 2 | Ulcers, able to eat solids |
| 3 | Ulcers, requires liquid diet only |
| 4 | Oral alimentation impossible |
Role of Patient Education in Mucositis Prevention
Educating patients promotes adherence to oral care protocols and timely reporting of symptoms. Provide instruction on:
- Proper brushing and rinsing techniques
- Recognizing early signs of mucositis
- When to seek medical attention
Distribute educational pamphlets and demonstrate care routines before treatment begins.
Integrating Multidisciplinary Care
Successful prevention of radiation-induced mucositis requires a collaborative effort among:
- Radiation oncologists
- Dentists and oral medicine specialists
- Dietitians
- Oncology nurses
- Pain management specialists
Preventing radiation therapy-induced mucositis demands a proactive, evidence-based, and patient-centered approach. By integrating rigorous oral hygiene practices, photobiomodulation therapy, cytoprotective agents, and nutritional support, we can significantly reduce the incidence and severity of mucositis, ensuring optimal patient outcomes and uninterrupted cancer treatment. A multidisciplinary framework remains pivotal in delivering comprehensive care.