Postoperative atrial fibrillation (POAF) is the most frequent arrhythmia following cardio-thoracic surgery, affecting 20–50% of patients undergoing coronary artery bypass grafting (CABG), valve replacements, or combined procedures. POAF is associated with prolonged hospital stays, increased risk of stroke, heightened mortality, and elevated healthcare costs. A comprehensive approach involving pharmacologic, non-pharmacologic, and surgical strategies is essential for its effective prevention.
Pathophysiology of Postoperative Atrial Fibrillation
POAF is a multifactorial phenomenon triggered by the interplay of systemic inflammation, oxidative stress, autonomic imbalance, electrolyte disturbances, and atrial ischemia. The physiological stress from sternotomy, pericardiotomy, and extracorporeal circulation creates a substrate conducive to arrhythmogenesis, particularly in patients with predisposing factors such as atrial enlargement or pre-existing conduction abnormalities.
Risk Factors for Post Cardio-Thoracic Surgery Atrial Fibrillation
- Age >65 years
- History of AF or supraventricular arrhythmias
- Hypertension and left atrial enlargement
- Chronic obstructive pulmonary disease (COPD)
- Diabetes mellitus and metabolic syndrome
- Prolonged cardiopulmonary bypass time
- Inflammatory states and oxidative stress markers
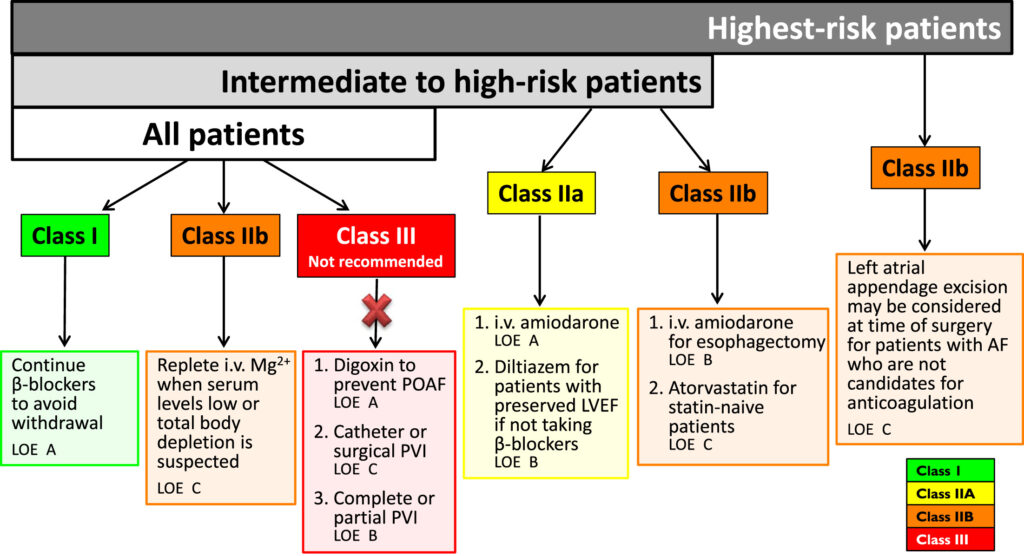
Pharmacological Prophylaxis for POAF Prevention
1. Beta-Blockers
Beta-blockers are the first-line pharmacologic agents for POAF prevention. Their efficacy lies in reducing sympathetic activation and stabilizing atrial electrical activity.
- Recommended initiation: 24 hours preoperatively or immediately postoperatively.
- Preferred agents: Metoprolol, atenolol, carvedilol.
- Contraindications: Severe bradycardia, AV block, acute decompensated heart failure.
2. Amiodarone
Amiodarone is highly effective for patients at high risk or when beta-blockers are contraindicated.
- Oral or IV administration: Preoperative loading dose (400–600 mg/day for 5–7 days), continued postoperatively for 5–7 days.
- Benefits: Suppresses atrial arrhythmias, minimal negative inotropic effects.
- Monitor for: Hepatotoxicity, thyroid dysfunction, pulmonary toxicity.
3. Sotalol
A hybrid beta-blocker and Class III antiarrhythmic agent offering rhythm stabilization.
- Initiate with caution due to risk of QT prolongation.
- Requires baseline and follow-up ECG monitoring.
4. Anti-inflammatory Agents
The inflammatory cascade post-surgery is a major contributor to POAF.
- Colchicine: Has shown efficacy in reducing POAF incidence by targeting pericardial inflammation.
- Corticosteroids: Useful in selected patients; however, routine use is limited due to adverse effects like infection and hyperglycemia.
Non-Pharmacological Measures to Reduce POAF Risk
1. Electrolyte Optimization
Maintaining optimal levels of potassium and magnesium reduces atrial excitability:
- Potassium > 4.0 mmol/L
- Magnesium > 2.0 mg/dL
Frequent monitoring is essential in the immediate postoperative period.
2. Maintaining Normothermia
Avoidance of hypothermia during surgery and rewarming phases helps stabilize the myocardial conduction system.
3. Minimizing Inflammatory Triggers
Reducing pericardial trauma, avoiding excessive use of electrocautery, and utilizing biocompatible bypass circuits can mitigate inflammation-related triggers.
4. Controlled Fluid Management
Preventing atrial stretch due to volume overload can reduce the mechanical predisposition to AF.
Surgical and Device-Based Approaches
1. Atrial Pacing
Temporary atrial pacing may prevent POAF by maintaining atrial conduction integrity and preventing bradyarrhythmia-related ectopy.
- Biatrial pacing is more effective than right atrial pacing alone.
- Indicated particularly in high-risk valve surgery patients.
2. Maze Procedure
In patients with a history of AF undergoing open heart surgery, the Cox-Maze III/IV procedure offers definitive rhythm control by creating conduction block lines.
- Adds surgical time but is highly effective in long-term sinus rhythm restoration.
Perioperative Monitoring and Early Detection
1. Continuous Telemetry
Continuous ECG monitoring in ICU and step-down units enables immediate detection and intervention in early episodes of AF.
2. Biomarker Surveillance
- C-reactive protein (CRP) and interleukin-6 (IL-6) serve as predictors of POAF risk.
- Monitoring may guide personalized anti-inflammatory prophylaxis.
Postoperative Management and Secondary Prevention
1. Rate vs. Rhythm Control
In persistent POAF beyond 48 hours, decision-making must balance patient stability, comorbidities, and stroke risk.
- Rate control: Beta-blockers, calcium channel blockers.
- Rhythm control: Cardioversion, continuation of amiodarone.
2. Anticoagulation Considerations
For episodes lasting more than 48 hours or recurrent AF:
- Initiate anticoagulation based on CHA₂DS₂-VASc score.
- Balance thromboembolism risk with bleeding potential, especially in the early postoperative phase.
Multimodal Prophylaxis: The Gold Standard
A tailored, multimodal prophylactic approach encompassing pharmacologic, electrolyte, pacing, and inflammatory control measures yields the highest success in minimizing POAF.
Preventing post cardio-thoracic surgery atrial fibrillation demands a robust, evidence-based, and patient-specific approach. By combining pharmacologic agents like beta-blockers and amiodarone with non-pharmacologic measures such as electrolyte management, inflammation reduction, and surgical pacing strategies, we can significantly reduce the incidence and impact of POAF. Continuous monitoring, individualized prophylaxis, and prompt intervention ensure optimal surgical outcomes and enhanced patient safety.