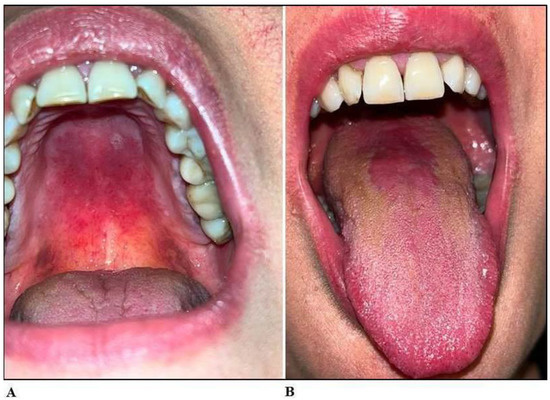
Oropharyngeal candidiasis, commonly referred to as oral thrush, is a fungal infection primarily caused by Candida albicans. It affects the mucous membranes of the mouth and throat, often presenting as white, curd-like plaques, erythema, and discomfort during swallowing. While it may occur in healthy individuals, it is most prevalent among immunocompromised patients, including those with HIV/AIDS, undergoing chemotherapy, organ transplantation, or corticosteroid therapy.
The prevention of oropharyngeal candidiasis is essential in reducing morbidity and improving the quality of life in at-risk populations.
High-Risk Populations for Oropharyngeal Candidiasis
- HIV/AIDS patients with low CD4 counts
- Cancer patients receiving chemotherapy or radiation
- Organ transplant recipients
- Inhaled corticosteroid users (e.g., for asthma or COPD)
- Dentures wearers, particularly those with poor oral hygiene
- Diabetic patients
- Infants and the elderly
Understanding the risk profile is critical in implementing personalized prevention strategies.
Antifungal Prophylaxis for Immunocompromised Patients
Pharmacologic Prophylaxis
Prophylactic antifungal medications are indicated in high-risk individuals to prevent colonization and progression to infection.
Commonly used agents:
- Fluconazole (oral): Preferred for systemic prophylaxis due to efficacy and tolerability.
- Clotrimazole troches: Effective for localized oropharyngeal use.
- Nystatin suspension: Often used in infants or mild cases.
Indications for Prophylaxis
- HIV patients with CD4 <200 cells/µL and recurrent thrush
- Hematopoietic stem cell transplant recipients
- Head and neck cancer patients undergoing radiotherapy
Prophylaxis should be tailored based on risk assessment, drug resistance potential, and individual tolerance.
Optimizing Oral Hygiene to Prevent Fungal Colonization
Daily Oral Care Practices
Maintaining proper oral hygiene significantly reduces the risk of oropharyngeal candidiasis, particularly in denture users and hospitalized patients.
Key measures:
- Brushing teeth twice daily with fluoride toothpaste
- Rinsing the mouth after meals and after using inhaled steroids
- Regular cleaning and disinfection of dentures
- Avoiding mouthwashes with high alcohol content
Denture Hygiene Protocol
- Remove dentures at night
- Soak in antifungal or disinfectant solution daily
- Brush dentures with a soft brush to remove biofilm
Immune System Support and Nutritional Considerations
Strengthening Host Defenses
Enhancing immune function is a cornerstone in preventing recurrent candidiasis.
- Antiretroviral therapy (ART) for HIV-positive individuals
- Glycemic control in diabetic patients
- Nutritional supplementation with iron, folate, and vitamin B12 as needed
Dietary Adjustments
Limiting refined sugars and fermentable carbohydrates may reduce fungal overgrowth. Probiotic-rich foods or supplements (e.g., Lactobacillus spp.) can help maintain microbial balance in the oral cavity.
Prevention in Patients Using Inhaled Corticosteroids
Proper Inhaler Technique and Rinsing
Inhaled corticosteroids are a common cause of iatrogenic oropharyngeal candidiasis. Preventive measures include:
- Using a spacer device with metered-dose inhalers
- Rinsing the mouth and throat with water and spitting after each use
- Minimizing the corticosteroid dose where clinically appropriate
Managing Recurrence and Resistance
Addressing Recurrent Infections
In patients experiencing frequent relapses, it is essential to reassess underlying causes such as immunosuppression, poor compliance, or antifungal resistance.
Stepwise approach:
- Identify and manage predisposing factors
- Consider antifungal susceptibility testing
- Rotate antifungal agents if resistance is suspected
Emerging Antifungal Resistance
Candida glabrata and Candida krusei exhibit reduced sensitivity to fluconazole. Echinocandins or amphotericin B may be necessary in such cases, especially in systemic infections.
The prevention of oropharyngeal candidiasis requires a proactive, multi-faceted approach. Effective prophylaxis in high-risk patients, rigorous oral hygiene, immune system support, and targeted pharmacologic strategies collectively minimize the risk of infection. By implementing individualized preventive protocols and staying alert to emerging resistance, we can ensure optimal oral health outcomes in vulnerable populations.