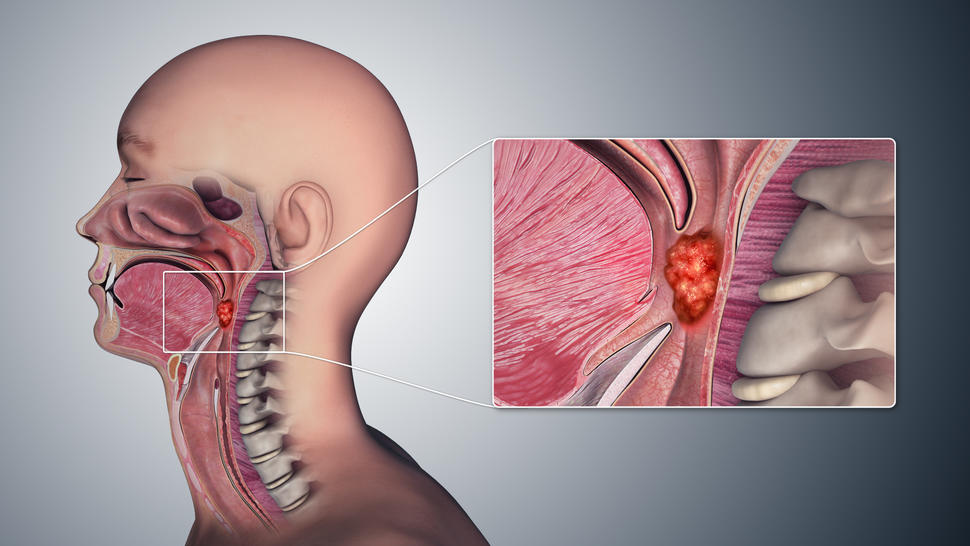
Oropharyngeal cancer, a malignancy affecting the middle part of the throat, has increasingly been linked to persistent infection with high-risk strains of human papillomavirus (HPV), particularly HPV-16. Unlike traditional risk factors such as tobacco and alcohol use, HPV-related oropharyngeal cancer often arises in younger, otherwise healthy individuals and is now one of the most rapidly rising cancers in high-income countries.
Effective prevention strategies must prioritize primary and secondary interventions, focusing on HPV transmission reduction, vaccination, and early detection.
Understanding the HPV-Oropharyngeal Cancer Connection
HPV is a sexually transmitted virus, with over 200 genotypes identified. Of these, HPV-16 is responsible for the majority of HPV-positive oropharyngeal squamous cell carcinomas. The virus infects epithelial tissues of the tonsils and base of the tongue, where it may evade immune detection and cause cellular changes leading to malignancy over several years.
HPV Vaccination: The Cornerstone of Prevention
Vaccines and Target Populations
The most effective preventive measure against HPV-associated oropharyngeal cancer is vaccination, which induces immunity before exposure to the virus.
Approved HPV vaccines:
- Gardasil 9 – covers 9 HPV types, including HPV-16 and HPV-18
- Gardasil (quadrivalent) – includes HPV-6, 11, 16, 18
- Cervarix (bivalent) – targets HPV-16 and 18
Recommended groups:
- Routine vaccination for boys and girls aged 9–12
- Catch-up vaccination up to age 26
- Select vaccination up to age 45 based on clinical judgment
Efficacy and Long-Term Impact
Studies have demonstrated near-complete protection against oral HPV infections in vaccinated individuals, with the potential to drastically reduce the incidence of oropharyngeal cancers over the coming decades.
Public Awareness and Education Initiatives
Addressing Vaccine Hesitancy
One of the most significant barriers to vaccine uptake is public misperception. Educational campaigns that emphasize the cancer-preventing potential of the HPV vaccine, rather than its link to sexual activity, have shown better community acceptance.
School and Community Programs
Integration of HPV education into school health curricula and community outreach programs ensures that adolescents and parents receive reliable, science-backed information about vaccination benefits.
Safe Sexual Practices to Reduce Oral HPV Transmission
Risk Reduction Strategies
Since HPV is transmitted via oral-genital contact, promoting safe sexual practices plays a vital role in reducing transmission:
- Consistent use of barrier protection (e.g., condoms, dental dams)
- Limiting number of sexual partners
- Open communication and HPV awareness among partners
While barrier methods do not eliminate risk entirely, they significantly reduce it.
Early Detection and Screening in High-Risk Populations
Identifying High-Risk Individuals
Routine screening for oropharyngeal cancer is not currently standard practice due to the lack of established screening tools. However, risk stratification can guide early evaluation:
- Men aged 35–65 with multiple lifetime oral sex partners
- Tobacco users with known HPV exposure
- HIV-positive individuals or those with immunosuppression
Clinical Surveillance
- Visual and tactile oral cavity exams during routine dental or ENT visits
- HPV DNA testing (emerging but not yet widely implemented)
- Biopsy of persistent oropharyngeal lesions or unexplained symptoms such as chronic sore throat or hoarseness
Health Policy and Global HPV Cancer Prevention Strategies
Integration Into National Immunization Programs
Countries with high HPV vaccination coverage have seen substantial reductions in HPV prevalence and precancerous lesions. Expanding national immunization programs to include both genders enhances herd immunity and broadens protection.
Policy-Driven Outcomes
- Australia is projected to eliminate cervical cancer in the next two decades due to aggressive HPV vaccination efforts.
- A parallel decline in HPV-positive oropharyngeal cancers is expected with similar strategies.
Research and Future Directions
Novel Screening Techniques
- Salivary biomarkers and oral HPV DNA testing are under investigation to enable non-invasive, early detection of HPV-related oropharyngeal cancers.
- Liquid biopsy approaches offer potential for monitoring recurrence and treatment response.
Therapeutic Vaccines
While current vaccines are preventive, therapeutic HPV vaccines are in development to treat existing infections and HPV-driven tumors, offering hope for individuals already affected.
Preventing oropharyngeal cancer due to human papillomavirus requires a comprehensive, multi-faceted strategy. Through widespread HPV vaccination, public education, responsible sexual behavior, and risk-targeted screening, we can significantly reduce the incidence of this increasingly prevalent cancer. As vaccine coverage grows and innovative screening technologies evolve, the global burden of HPV-associated oropharyngeal cancer is poised to decline, securing better long-term outcomes for future generations.

