Group B Streptococcus (Streptococcus agalactiae, GBS) is a leading cause of severe infections in newborns, including sepsis, pneumonia, and meningitis. GBS is typically found in the lower gastrointestinal and genitourinary tracts of healthy adults and may be vertically transmitted from mother to child during labor or delivery.
Two clinical forms are recognized:
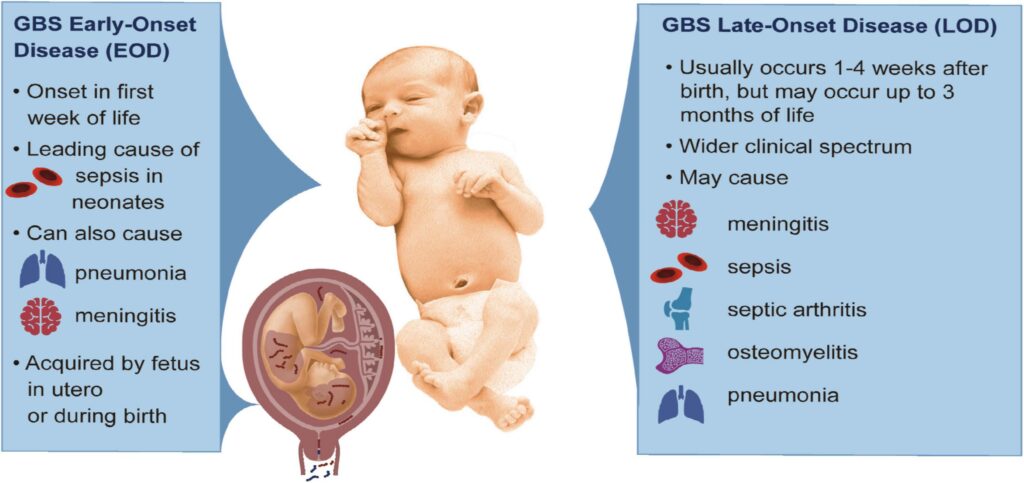
- Early-onset GBS disease (EOGBSD): Occurs within the first 7 days of life, usually within 24 hours.
- Late-onset GBS disease: Occurs from 7 days to 3 months after birth and is less associated with delivery-related transmission.
Effective prevention of EOGBSD is paramount due to its rapid onset and potential fatality.
Risk Factors for Neonatal GBS Infection
Identifying maternal and perinatal risk factors is essential for targeted prevention:
- GBS colonization in the mother (vaginal or rectal)
- Preterm labor (<37 weeks)
- Prolonged rupture of membranes (>18 hours)
- Intrapartum fever (≥100.4°F / 38°C)
- Previous infant with GBS disease
- Positive GBS bacteriuria during current pregnancy
Universal Screening and Culture-Based Protocols
Maternal GBS Screening at 36–37 Weeks’ Gestation
We advocate universal vaginal-rectal screening using culture techniques during 36–37 weeks of gestation. This timeframe optimizes detection of maternal colonization at the time of delivery.
Laboratory protocol:
- Swab both vaginal introitus and rectum
- Culture using selective enrichment broth (e.g., Lim broth)
- Identification and antibiotic susceptibility testing for penicillin-allergic patients
Intrapartum Antibiotic Prophylaxis (IAP)
Primary Preventive Measure Against Early-Onset GBS Disease
Intrapartum antibiotic prophylaxis (IAP) is the cornerstone of prevention. It is administered during labor to reduce neonatal exposure to GBS.
Indications for IAP:
- Positive GBS culture
- GBS bacteriuria during pregnancy
- Previous infant with GBS disease
- Unknown GBS status and any of the following:
- Preterm labor
- Intrapartum fever
- Prolonged membrane rupture
Recommended Regimens:
| Maternal Status | Antibiotic | Dosage |
|---|---|---|
| GBS-positive, no allergy | Penicillin G | 5 million units IV initial, then 2.5–3 million units IV every 4 hours |
| Mild penicillin allergy | Cefazolin | 2 g IV initial, then 1 g IV every 8 hours |
| High-risk penicillin allergy | Clindamycin (if susceptible) | 900 mg IV every 8 hours |
| Resistant or unknown susceptibility | Vancomycin | 1 g IV every 12 hours |
IAP should begin at least 4 hours before delivery for optimal neonatal protection.
Strategies for Penicillin-Allergic Patients
Assessment of penicillin allergy severity is crucial to select appropriate antibiotics:
- Low-risk allergies (e.g., rash): Cefazolin is generally safe.
- High-risk allergies (e.g., anaphylaxis): Use clindamycin if the isolate is susceptible, or vancomycin if not.
GBS isolates should be tested for resistance, particularly to clindamycin and erythromycin, due to increasing resistance rates.
Role of Rapid Diagnostic Testing
In settings where culture results are unavailable at delivery, rapid intrapartum NAATs (nucleic acid amplification tests) can identify maternal colonization within hours.
Benefits include:
- Real-time GBS detection
- Reduced unnecessary antibiotic use
- Enhanced targeting in cases with unknown status
However, access, cost, and lab capacity may limit routine use.
Management of Preterm Labor and Premature Rupture of Membranes
Preterm births pose a higher GBS transmission risk. In these cases:
- If culture status is unknown, administer IAP based on risk factors
- If previously GBS-positive, proceed with IAP regardless of gestational age
- Consider corticosteroids and tocolytics to improve neonatal outcomes while IAP is administered
Neonatal Evaluation and Management After Birth
Newborns of Mothers Who Received IAP
If IAP was administered adequately (≥4 hours before delivery), and the infant is asymptomatic:
- Routine newborn care
- No further evaluation unless clinical signs develop
Newborns Without Adequate IAP
If the mother received inadequate or no IAP and the infant is well-appearing:
- Monitor for ≥48 hours
- Blood cultures may be considered based on clinical judgment
If the newborn is symptomatic:
- Immediate evaluation with blood cultures
- Initiation of empiric antibiotics (e.g., ampicillin + gentamicin)
Future Directions: Maternal GBS Vaccination
Several candidate vaccines are in development to prevent maternal colonization and subsequent neonatal transmission. A successful maternal GBS vaccine would:
- Provide immunity prior to delivery
- Potentially eliminate the need for IAP
- Reduce late-onset GBS disease
Global implementation remains pending the results of ongoing trials and regulatory approvals.
Summary Table: GBS Prevention Guidelines
| Strategy | Recommendation |
|---|---|
| Universal screening | At 36–37 weeks gestation |
| IAP candidates | GBS-positive, previous GBS infant, GBS bacteriuria |
| IAP timing | Start ≥4 hours before delivery |
| First-line antibiotic | Penicillin G |
| Allergy alternatives | Cefazolin, Clindamycin, Vancomycin |
| Neonatal management | Observe or evaluate based on IAP status and symptoms |
| Vaccine development | Promising but not yet standard |
The prevention of neonatal Group B Streptococcal infection hinges on timely maternal screening, appropriate intrapartum antibiotic administration, and vigilant newborn monitoring. Adhering to current guidelines dramatically reduces the risk of early-onset disease and associated morbidity. With emerging vaccine research, we may soon witness a paradigm shift in the long-term control of GBS transmission.