Meningococcal meningitis is a severe bacterial infection caused by Neisseria meningitidis, which inflames the protective membranes surrounding the brain and spinal cord. Despite advancements in treatment, the disease poses a high risk of mortality and long-term complications if not prevented effectively. Outbreaks occur globally, particularly in areas with limited access to vaccines and healthcare infrastructure.
Primary Prevention Through Vaccination
Importance of Meningococcal Vaccines
Vaccination remains the cornerstone of meningococcal meningitis prevention. Multiple vaccines target various serogroups of Neisseria meningitidis:
- MenACWY: Protects against serogroups A, C, W, and Y.
- MenB: Specifically targets serogroup B, common in infants and young adults.
- MenAfriVac: A cost-effective vaccine used in the African meningitis belt to eliminate group A meningitis.
National immunization programs in many countries include routine adolescent vaccination with boosters. For high-risk populations—such as immunocompromised individuals, travelers to endemic areas, and university students—vaccination is strongly advised.
Recommended Vaccination Schedules
- Infants (under 1 year): MenB series starting at 2 months (as per local guidelines).
- Adolescents (11–12 years): MenACWY with a booster at age 16.
- Adults at risk: As advised by healthcare providers, especially for military recruits, lab workers, and travelers.
Early Identification and Prompt Intervention
Recognizing Symptoms Early
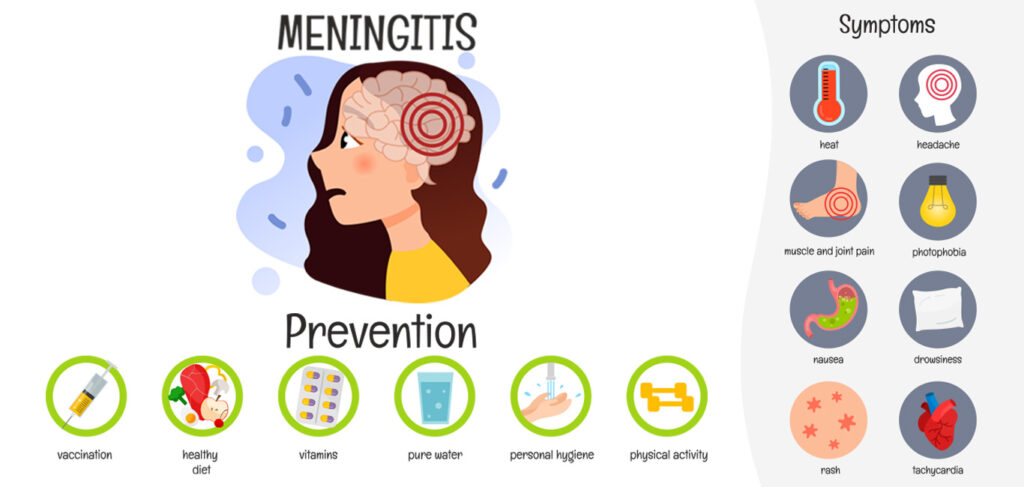
Timely identification of symptoms allows for rapid medical intervention. Key signs of meningococcal meningitis include:
- Sudden high fever
- Stiff neck
- Headache
- Photophobia
- Altered mental status
- Vomiting and seizures
In infants, symptoms may include poor feeding, irritability, and a bulging fontanelle.
Immediate Medical Response
Suspected cases should be treated as medical emergencies. Intravenous antibiotics, corticosteroids, and supportive care are critical to reduce mortality and mitigate complications such as hearing loss, cognitive deficits, and limb amputation.
Public Health Measures to Prevent Outbreaks
Surveillance and Case Reporting
Robust epidemiological surveillance systems are essential. Prompt identification and reporting allow health authorities to initiate outbreak control measures, including targeted vaccination campaigns and prophylaxis for close contacts.
Chemoprophylaxis for Close Contacts
Close contacts of infected individuals should receive prophylactic antibiotics, such as rifampin or ciprofloxacin, within 24 hours of case detection. This reduces the risk of secondary transmission, especially in household or school settings.
Hygienic Practices and Environmental Control
Reducing Transmission Through Hygiene
Transmission occurs through respiratory droplets and close contact. Preventive measures include:
- Frequent handwashing
- Avoiding sharing eating utensils and drinks
- Covering mouth and nose when sneezing
- Isolating infected individuals during the infectious period
Enhancing Ventilation and Reducing Overcrowding
Crowded environments such as dormitories and refugee camps facilitate outbreaks. Ensuring proper ventilation and spacing can reduce risk, particularly in endemic regions.
Special Considerations for Travelers and High-Risk Groups
Travel to Endemic Regions
Individuals traveling to areas with frequent outbreaks, such as the African meningitis belt (from Senegal to Ethiopia), must be vaccinated at least 10 days before travel. Proof of vaccination is often required for entry during high-risk seasons.
Vulnerable Populations
Special attention must be given to:
- Individuals with asplenia or complement deficiencies
- People with HIV/AIDS
- Laboratory workers handling Neisseria meningitidis
- College students in dormitories and military recruits
Routine screening and vaccination are essential for these groups.
Global Initiatives and the Role of WHO
The Defeating Meningitis Roadmap
The World Health Organization’s “Defeating Meningitis by 2030” initiative outlines a global strategy to reduce meningitis incidence and deaths through:
- Expanded access to vaccination
- Improved diagnostics
- Strengthened surveillance
- Increased public awareness
Collaborative Research and Vaccine Development
Continued research into broad-spectrum meningococcal vaccines remains a priority. The development of affordable, multivalent vaccines is critical for long-term global prevention, especially in low-income countries.
Educational Campaigns and Community Involvement
Raising Awareness
Educational campaigns in schools, colleges, and community centers ensure that individuals recognize the signs of meningitis and the importance of vaccination.
Community Health Workers
Trained community health workers play a vital role in outbreak prevention by disseminating accurate information, identifying symptomatic individuals, and facilitating access to healthcare and immunization.
Preventing meningococcal meningitis requires a multi-faceted approach, with vaccination at its core. Vigilant surveillance, public health interventions, personal hygiene, and rapid medical response collectively reduce the risk of outbreaks and fatalities. International cooperation and local education further enhance prevention efforts, aligning with global goals to defeat meningitis in the coming decade.