Measles remains a highly contagious viral illness with significant public health implications. Prompt and evidence-based intervention following exposure is essential to prevent transmission and limit outbreaks. Implementing robust post-exposure prophylaxis (PEP) strategies is critical in high-risk settings such as schools, healthcare facilities, and communities with low vaccination coverage.
Understanding Measles Transmission Dynamics
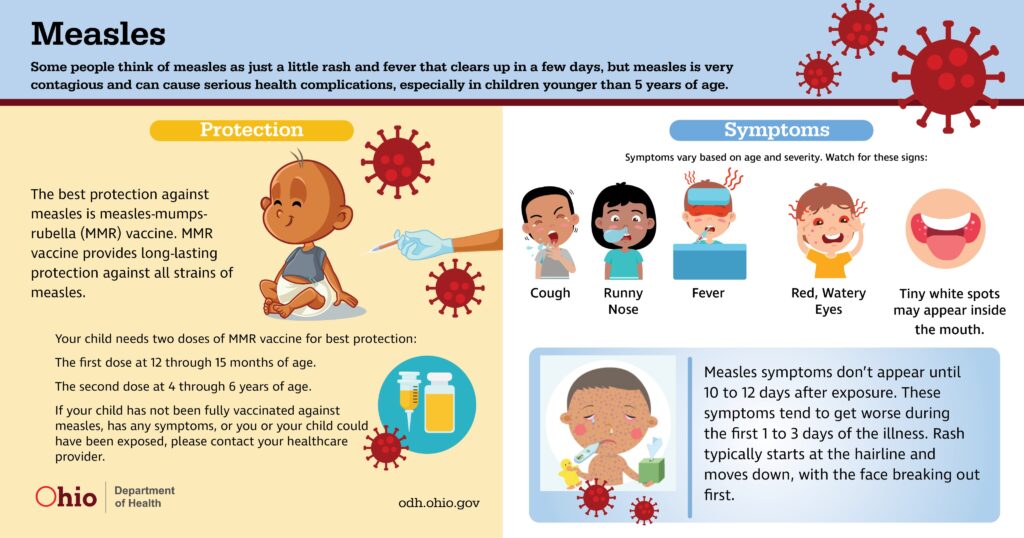
Measles is caused by the Measles morbillivirus, transmitted primarily through respiratory droplets. The virus can remain airborne and infectious for up to two hours in enclosed spaces. The incubation period typically ranges from 7 to 14 days, with individuals becoming contagious approximately 4 days before and after rash onset.
Immediate Response Following Measles Exposure
Identify and Evaluate Exposed Individuals
A thorough assessment of exposed persons is the first step:
- Determine immune status (vaccination history, serologic evidence)
- Assess time since exposure
- Identify high-risk groups: infants, pregnant individuals, immunocompromised patients, unvaccinated adults
Prompt classification allows for targeted intervention.
MMR Vaccine as Post-Exposure Prophylaxis
Administering the MMR Vaccine Within 72 Hours
The measles-mumps-rubella (MMR) vaccine is the first line of defense when administered within 72 hours of exposure to a susceptible individual.
Key Guidelines:
- Indicated for unvaccinated or partially vaccinated persons
- Contraindicated in pregnancy and immunocompromised states
- Not effective after 72 hours, but still beneficial for long-term immunity
MMR vaccine post-exposure can either prevent the disease entirely or reduce the severity of symptoms.
Immune Globulin (IG) Administration for High-Risk Populations
Use of IG Within 6 Days of Exposure
For individuals who cannot receive the MMR vaccine, immune globulin (IG) offers passive immunity and should be administered within 6 days of exposure.
Indications for IG:
- Infants <6 months of age
- Pregnant women without immunity
- Severely immunocompromised individuals
Dosage Forms:
- Intramuscular IG (IGIM): For most susceptible individuals
- Intravenous IG (IGIV): For severely immunocompromised patients
Timely IG administration significantly reduces the likelihood of symptomatic infection.
Quarantine and Isolation Protocols
Containing Potential Spread
Public health authorities must implement strict containment measures to prevent further transmission.
Isolation:
- Individuals diagnosed with measles must be isolated for 4 days after rash onset
- Airborne precautions are essential in healthcare settings
Quarantine:
- Non-immune individuals should be excluded from public settings (e.g., schools, daycare) from day 5 through day 21 post-exposure
- Immediate PEP can modify or negate the need for full quarantine if effective
Special Considerations for Healthcare Settings
Healthcare workers exposed to measles must be rapidly assessed:
- Documented immunity (two doses of MMR or serologic evidence) eliminates the need for PEP
- Non-immune workers should receive MMR within 72 hours or IG if contraindicated
- Infected staff must remain off duty from day 5 through day 21 after exposure or until 4 days post-rash if infected
Measles Surveillance and Contact Tracing
Critical Role of Public Health Infrastructure
Effective measles control requires:
- Timely reporting of confirmed or suspected cases
- Comprehensive contact tracing to identify and assess all exposed individuals
- Vaccination campaigns in under-immunized communities to raise herd immunity
These efforts help break the transmission chain and prevent outbreaks.
High-Risk Populations and Tailored PEP Guidelines
Infants:
- <6 months: IGIM preferred
- 6–11 months: MMR may be given as an early dose (does not count toward routine vaccination)
Pregnant Women:
- Contraindicated for MMR
- IGIM strongly recommended if exposed and non-immune
Immunocompromised Individuals:
- Cannot receive live vaccines
- Require IGIV for adequate protection
Recommendations for Schools and Public Institutions
- Verify MMR immunity documentation for staff and students
- Maintain vaccination records for immediate access during outbreaks
- Enforce exclusion policies for exposed, non-immune individuals
- Conduct educational campaigns to improve vaccination coverage
Long-Term Prevention Through Vaccination
Preventing measles outbreaks depends on maintaining high vaccination coverage:
- Two doses of MMR vaccine are 97% effective against measles
- Community immunity thresholds require ≥95% vaccination coverage
- Immunization drives must target underserved and vaccine-hesitant populations
Frequently Asked Questions
Can measles be prevented after exposure?
Yes, with timely MMR vaccination within 72 hours or immune globulin within 6 days, measles can often be prevented or mitigated.
Who needs immune globulin after measles exposure?
High-risk individuals such as infants, pregnant women, and immunocompromised patients should receive immune globulin if exposed.
Is quarantine mandatory after measles exposure?
Yes, for unvaccinated individuals who decline PEP or receive it too late. Quarantine helps prevent community spread.
Can I receive the MMR vaccine during an outbreak even if I’m unsure of past doses?
Yes. There’s no harm in receiving an additional dose, and it ensures protection during outbreaks.
How soon should I act after exposure?
Immediate action is critical. The first 72 hours post-exposure is the ideal window for vaccination, and within 6 days for IG administration.
The prevention of measles after exposure hinges on swift identification, targeted prophylaxis, and stringent public health measures. Administering MMR vaccine within 72 hours or immune globulin within 6 days can significantly reduce transmission risk. Coupled with effective quarantine, surveillance, and vaccination policies, these strategies form the foundation for robust measles outbreak control and long-term eradication goals.