Invasive pulmonary aspergillosis (IPA) is a life-threatening fungal infection predominantly affecting immunocompromised individuals, particularly those with hematologic malignancies, prolonged neutropenia, or solid organ transplants. Effective prevention of IPA is vital in reducing morbidity and mortality among these vulnerable patient groups.
Understanding Invasive Pulmonary Aspergillosis and Its Risk Profile
IPA is caused by Aspergillus species, ubiquitous mold fungi found in the environment. The most common pathogen is Aspergillus fumigatus. Spores, when inhaled, can colonize and invade lung tissue, especially in hosts with weakened immune defenses.
High-Risk Groups:
- Patients undergoing hematopoietic stem cell transplantation (HSCT)
- Individuals with acute myeloid leukemia (AML) or other hematologic cancers
- Patients on prolonged corticosteroid therapy
- Solid organ transplant recipients
- Severe prolonged neutropenia (<500 cells/µL for >10 days)
- Intensive care unit patients with COVID-19-associated pulmonary aspergillosis (CAPA)
Environmental Controls to Limit Aspergillus Exposure
1. HEPA Filtration in Healthcare Settings
High-efficiency particulate air (HEPA) filters are crucial in removing airborne spores from patient environments.
- HEPA filters remove ≥99.97% of particles ≥0.3 μm, including fungal spores
- Recommended in protective isolation rooms for neutropenic patients
- Regular maintenance and positive pressure airflow systems enhance efficacy
2. Construction and Renovation Safeguards
Construction work increases airborne spore counts significantly.
- Implement barriers and negative pressure zones near construction areas
- Use moisture control to prevent mold growth in hospital infrastructure
- Staff and patients should avoid construction areas during active work
3. Routine Cleaning Protocols
Fungal spores can colonize dust and debris.
- Use hospital-grade sporicidal disinfectants
- Clean ventilation systems regularly
- Limit the presence of potted plants, flowers, and wood-based materials in high-risk units
Antifungal Prophylaxis: Pharmacological Prevention Strategies
1. Triazole Antifungals
Triazoles are the cornerstone of IPA prophylaxis.
Posaconazole (preferred agent):
- Recommended in patients with prolonged neutropenia or GVHD
- Oral delayed-release tablets: 300 mg once daily after loading dose
Voriconazole and Itraconazole are alternatives, though they may have variable bioavailability and drug-drug interactions.
2. Echinocandins and Amphotericin B
Used when triazoles are contraindicated.
- Micafungin or Caspofungin can be used in HSCT recipients intolerant to azoles
- Liposomal amphotericin B reserved for patients with breakthrough infections or resistance
3. Therapeutic Drug Monitoring (TDM)
Essential for ensuring efficacy and minimizing toxicity.
- Voriconazole trough level target: 1–5.5 µg/mL
- Adjust dosages based on TDM results and hepatic function
Host Factor Optimization to Minimize Susceptibility
1. Neutropenia Management
- Administer G-CSF (Granulocyte-Colony Stimulating Factor) in chemotherapy-induced neutropenia
- Monitor ANC trends to guide antifungal initiation and escalation
2. Immunosuppressive Therapy Modulation
- Minimize use and duration of systemic corticosteroids
- Adjust immunosuppressants post-transplant based on infection risk
3. Vaccination and Immune Recovery
While no vaccine exists for aspergillosis, supporting general immune reconstitution reduces the risk of opportunistic infections.
Diagnostic Surveillance and Early Detection Measures
1. Galactomannan Testing
- Performed on serum or bronchoalveolar lavage (BAL) fluid
- Helps detect fungal antigens before clinical symptoms arise
- Weekly screening in high-risk patients is advised
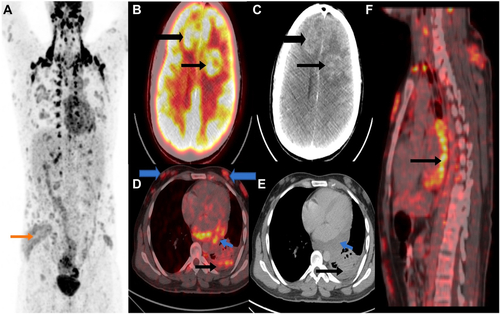
2. Aspergillus PCR and Imaging
- Aspergillus DNA PCR assays provide rapid diagnostic information
- High-resolution CT often shows halo sign or air crescent sign in early IPA
3. Biomarker-Based Risk Stratification
Combined use of biomarkers (galactomannan, beta-D-glucan) enhances specificity for IPA prediction and early therapy initiation.
Institutional Protocol Recommendations
CDC and IDSA Guidelines
- Posaconazole prophylaxis in patients with AML/MDS during induction chemotherapy
- Emphasis on environmental controls in transplant units
- Implementation of clinical pathways to ensure early intervention and monitoring
ECIL (European Conference on Infections in Leukaemia)
- Strong support for TDM in triazole therapy
- Advocates for multi-modal diagnostic tools in surveillance
- Calls for individualized risk stratification based on patient and treatment profiles
Frequently Asked Questions:
What is invasive pulmonary aspergillosis?
IPA is a serious fungal infection caused by Aspergillus species, primarily affecting the lungs of immunocompromised individuals.
Who is most at risk for IPA?
Patients undergoing chemotherapy, stem cell transplants, or receiving long-term corticosteroids are at the highest risk.
How is IPA prevented?
Prevention includes antifungal prophylaxis (usually triazoles), HEPA-filtered environments, routine surveillance, and minimizing immunosuppression.
Can IPA be fatal?
Yes. IPA has a high mortality rate, often exceeding 50%, especially when diagnosis or treatment is delayed.
Is there a vaccine for aspergillosis?
No vaccines are currently available. Prevention focuses on exposure reduction and antifungal prophylaxis.
Preventing invasive pulmonary aspergillosis requires a comprehensive, multidisciplinary approach combining environmental controls, antifungal prophylaxis, host optimization, and early diagnostic surveillance. Through strict adherence to evidence-based protocols and continuous risk assessment, healthcare providers can significantly mitigate the burden of IPA in high-risk populations.