Transrectal ultrasound-guided (TRUS) prostate biopsy remains a cornerstone in prostate cancer diagnosis. However, due to the anatomical proximity of the rectum, this procedure carries a substantial risk of post-biopsy infection, including urinary tract infections (UTIs), prostatitis, and sepsis. With rising fluoroquinolone-resistant organisms, the need for robust preventive strategies is paramount.
Infection Pathophysiology in Transrectal Prostate Biopsy
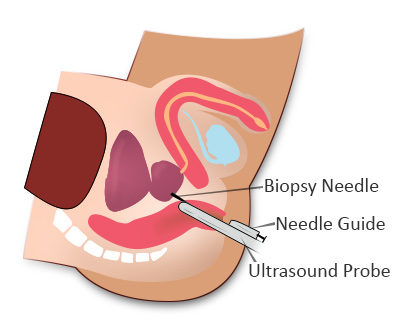
During TRUS-guided biopsy, the needle passes through the rectal mucosa into the prostate. This route provides a direct pathway for enteric flora, including Escherichia coli, to enter sterile urinary and prostatic tissues. The resulting complications may range from mild lower urinary tract symptoms to severe urosepsis.
Key routes of microbial entry:
- Breach of the rectal wall during needle insertion
- Inadequate rectal preparation
- Contamination of biopsy instruments
- Colonization by fluoroquinolone-resistant bacteria
Risk Factors for Post-Biopsy Infection
Identifying high-risk individuals is critical for tailoring infection prevention strategies. Major risk factors include:
- Recent antibiotic use (especially fluoroquinolones)
- Travel history to regions with high resistance rates
- History of prostatitis or UTI
- Diabetes mellitus or immunosuppression
- Indwelling urinary catheter
- Inadequate bowel preparation
Pre-Biopsy Strategies for Infection Prevention
1. Rectal Swab for Culture-Directed Antibiotic Prophylaxis
Obtaining a rectal swab culture 3–5 days prior to biopsy allows identification of resistant organisms, enabling targeted antibiotic selection.
- Cultures should screen for extended-spectrum beta-lactamase (ESBL) producers and fluoroquinolone resistance
- Tailored antibiotics significantly reduce post-biopsy sepsis rates compared to empirical prophylaxis
2. Antibiotic Prophylaxis Protocol
Empirical antibiotic prophylaxis has been standard; however, its effectiveness is diminishing due to resistant strains.
Recommended approach:
- Single-dose prophylaxis, administered 30–60 minutes before biopsy
- Common regimens:
- Ciprofloxacin 500 mg PO or Levofloxacin 500 mg PO
- Gentamicin IV/IM added in high-risk or known resistant cases
- Third-generation cephalosporins for ESBL carriers
Avoid prolonged courses unless clinical symptoms arise post-biopsy.
3. Mechanical Bowel Preparation
Cleansing the rectum reduces the bacterial load and risk of needle contamination.
Protocols may include:
- Self-administered fleet enema 2 hours before biopsy
- Bisacodyl suppository the night before
- Clear liquid diet 12–24 hours prior to procedure
Aseptic Technique During Biopsy
1. Sterile Field and Equipment Handling
- Use of sterile probe covers and biopsy needles
- Double gloving technique to prevent cross-contamination
- Apply antiseptic lubricant during probe insertion
2. Rectal Disinfection
Pre-insertion rectal cleansing with 10% povidone-iodine solution has demonstrated reduction in post-biopsy infections.
- Apply antiseptic to the rectal vault 5–10 minutes before procedure
- Consider reapplication for multiple biopsy cores or prolonged procedures
Post-Biopsy Care and Surveillance
1. Observation and Symptom Monitoring
Patients should be observed for 24–72 hours post-procedure for signs of infection:
- Fever ≥38°C
- Dysuria or increased urinary frequency
- Hematuria or rectal bleeding
- General malaise or rigors
Early identification facilitates prompt treatment of emerging infections.
2. Patient Education
Educate patients to promptly report:
- Fever or chills within a week post-biopsy
- Painful urination or cloudy urine
- Severe rectal bleeding or difficulty voiding
Provide written instructions and 24/7 contact information for emergency consultation.
Alternatives to Transrectal Approach
Given infection risks, some institutions are shifting toward transperineal prostate biopsy, which bypasses the rectal mucosa entirely.
Advantages include:
- Lower infection rates
- No need for rectal disinfection
- Feasible under local anesthesia with modern grid-based systems
However, wider adoption is limited by logistical constraints and training requirements.
International Guidelines and Recommendations
American Urological Association (AUA)
- Advocates risk-based antibiotic selection
- Supports use of rectal antiseptic preparation
- Endorses transperineal biopsy where feasible
European Association of Urology (EAU)
- Recommends culture-directed prophylaxis as first-line strategy
- Encourages research into alternative biopsy routes
- Advises limiting fluoroquinolone use in high-resistance areas
Frequently Asked Questions:
What is the infection rate after a transrectal prostate biopsy?
Reported infection rates vary from 1% to 7%, with sepsis occurring in <1% of cases when appropriate prophylaxis is used.
Which antibiotic is best for prostate biopsy?
Fluoroquinolones like ciprofloxacin are commonly used, but culture-based regimens with cephalosporins or aminoglycosides are increasingly favored.
Is bowel preparation necessary?
Yes. A fleet enema or suppository reduces rectal bacterial load, minimizing the chance of infection.
Can prostate biopsy cause sepsis?
Yes, although rare, post-biopsy sepsis is a life-threatening complication and must be promptly treated.
Are there safer alternatives to the transrectal biopsy?
Transperineal biopsy offers a significantly reduced infection risk and is becoming more common in many centers.
Preventing infection in transrectal prostate biopsy requires a multifaceted approach, integrating microbiological surveillance, antibiotic stewardship, mechanical bowel prep, and stringent aseptic technique. With antibiotic resistance on the rise, shifting to targeted prophylaxis and exploring alternative biopsy routes will remain central to safeguarding patient health and optimizing procedural outcomes.