Glucocorticoid-induced osteoporosis (GIOP) is the most common form of secondary osteoporosis and a significant cause of morbidity among patients receiving long-term corticosteroid therapy. Effective prevention and management of GIOP are essential for reducing fracture risk and preserving bone health. We present current clinical guidelines, pharmacological strategies, and lifestyle interventions aimed at mitigating glucocorticoid-related bone loss.
Pathophysiology of Glucocorticoid-Induced Osteoporosis
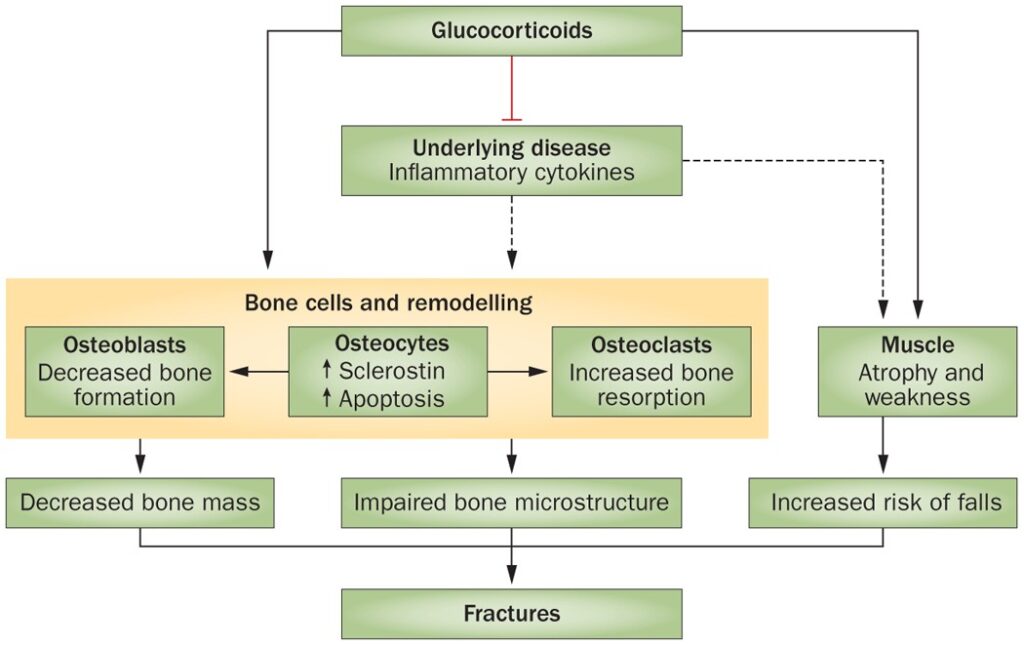
Glucocorticoids adversely affect bone metabolism through multiple mechanisms:
- Reduced osteoblast function: Suppression of bone formation
- Enhanced osteoclast activity: Accelerated bone resorption
- Calcium metabolism disruption: Decreased gastrointestinal absorption and increased renal excretion
- Sex hormone suppression: Reduced levels of estrogen and testosterone
The result is rapid bone loss, particularly in the trabecular-rich regions such as the spine and ribs, often occurring within the first 3–6 months of glucocorticoid initiation.
Identifying Patients at Risk
Risk Factors for GIOP
- Glucocorticoid dose ≥5 mg/day of prednisone (or equivalent) for ≥3 months
- Postmenopausal women and men over 50
- History of fragility fractures
- Low baseline bone mineral density (BMD)
- Concurrent use of medications affecting bone metabolism (e.g., proton pump inhibitors, anticonvulsants)
Bone Mineral Density Assessment
Dual-energy X-ray absorptiometry (DXA) is the standard for assessing BMD. Testing should be performed at:
- Baseline (before or at the start of glucocorticoid therapy)
- 6–12 months after initiation
- Every 1–2 years thereafter, depending on risk factors and treatment status
Pharmacological Prevention Strategies
Calcium and Vitamin D Supplementation
- Calcium: 1,000–1,200 mg/day (preferably from dietary sources)
- Vitamin D3 (cholecalciferol): 800–1,000 IU/day, or higher if deficient
These are foundational interventions for all patients receiving chronic glucocorticoid therapy.
Bisphosphonates
Bisphosphonates are first-line agents for the prevention and treatment of GIOP due to their ability to inhibit osteoclast-mediated bone resorption.
| Drug Name | Typical Dose | Notes |
|---|---|---|
| Alendronate | 70 mg once weekly (oral) | Avoid in patients with esophageal issues |
| Risedronate | 35 mg once weekly (oral) | Food intake interferes with absorption |
| Zoledronic Acid | 5 mg once yearly (IV infusion) | Useful in patients with poor compliance |
Initiation is recommended in:
- Adults ≥40 years on ≥7.5 mg/day prednisone for ≥3 months
- Younger patients with fracture history or low BMD
Other Agents for Specific Populations
- Teriparatide: Reserved for high-risk patients or those intolerant to bisphosphonates
- Denosumab: An alternative for postmenopausal women with high fracture risk
- Hormone replacement therapy (HRT): Considered in younger women with hormone deficiency
Lifestyle and Non-Pharmacological Measures
Physical Activity
- Weight-bearing and resistance exercises improve bone density and reduce fall risk
- Activities should be tailored to the patient’s mobility and fracture risk
Fall Prevention
- Home safety assessments
- Vision correction
- Balance training
- Medication review to reduce sedatives
Nutrition
- High-protein diet with adequate magnesium, phosphorus, and vitamin K
- Limit alcohol and caffeine
- Stop smoking, which independently increases fracture risk
Monitoring and Follow-Up
Bone Health Surveillance
- Repeat DXA scans every 12–24 months
- Biochemical markers (e.g., serum CTX, P1NP) can monitor treatment response
Glucocorticoid Therapy Review
- Use the lowest effective dose for the shortest duration
- Explore glucocorticoid-sparing agents (e.g., methotrexate, biologics)
- Taper off therapy gradually under medical supervision
Guidelines from Major Health Organizations
- American College of Rheumatology (ACR): Recommends initiating bisphosphonates in adults over 40 on ≥2.5 mg/day prednisone for >3 months
- National Osteoporosis Foundation (NOF): Supports routine DXA screening and supplementation for all long-term steroid users
- Endocrine Society: Suggests teriparatide in patients with severe osteoporosis or intolerance to other agents
Frequently Asked Questions
When should treatment for GIOP be initiated?
Prophylactic treatment should begin simultaneously with the start of long-term glucocorticoid therapy, particularly if the dose exceeds 5–7.5 mg/day for more than 3 months.
Can short-term steroid use cause osteoporosis?
Even short-term therapy can cause rapid bone loss, especially in high-risk individuals. Preventive measures should be considered if steroids are repeated or prolonged.
What if a patient cannot tolerate oral bisphosphonates?
Intravenous zoledronic acid or denosumab are suitable alternatives. Teriparatide is considered for very high-risk patients or in case of multiple fractures.
Is bone loss reversible after stopping glucocorticoids?
Some recovery of bone mass is possible, but full reversal may not occur, especially in older adults or those with multiple risk factors.
How long should bisphosphonates be continued?
For 3–5 years, depending on fracture risk, after which reassessment is warranted. Drug holidays may be considered in low-risk individuals.
Preventing glucocorticoid-induced osteoporosis requires a proactive, evidence-based approach encompassing pharmacological therapy, dietary optimization, physical activity, and regular monitoring. By adhering to clinical guidelines and tailoring interventions to individual risk profiles, we can effectively safeguard skeletal health and reduce the long-term burden of corticosteroid therapy.