Cytomegalovirus (CMV) is a widespread herpesvirus with the potential to cause severe disease in immunocompromised individuals, including organ transplant recipients, HIV-infected patients, and newborns infected in utero. While typically asymptomatic in healthy individuals, CMV reactivation or primary infection in vulnerable hosts can result in life-threatening organ involvement, graft rejection, or congenital complications. The prevention of cytomegalovirus disease is therefore a vital aspect of medical care in these settings, combining screening protocols, antiviral prophylaxis, and immune monitoring.
Understanding Cytomegalovirus: Risk and Transmission
CMV is a double-stranded DNA virus that establishes lifelong latency following primary infection. Transmission occurs through:
- Direct contact with infected body fluids (saliva, urine, semen, breast milk)
- Blood transfusion and organ transplantation
- Vertical transmission from mother to fetus
The virus remains dormant but can reactivate when host immunity weakens, especially in patients undergoing immunosuppressive therapy.
High-Risk Groups for CMV Disease
Effective CMV prevention strategies target populations at elevated risk:
- Solid Organ Transplant (SOT) Recipients
- Hematopoietic Stem Cell Transplant (HSCT) Recipients
- HIV-Infected Individuals with Low CD4+ Counts
- Pregnant Women and Neonates
- Patients Receiving Intensive Immunosuppression
Each group requires a tailored approach based on CMV serostatus, immunosuppressive burden, and exposure risk.
CMV Screening and Risk Stratification
CMV serology (IgG/IgM) and polymerase chain reaction (PCR) testing play a central role in identifying at-risk individuals and guiding preventive measures.
Pre-Transplant Screening
- Donor and Recipient CMV IgG status should be assessed prior to transplant.
- D+/R− (donor positive, recipient negative) is the highest risk configuration for post-transplant CMV disease.
Maternal and Neonatal Screening
- Pregnant women are screened for CMV IgG/IgM.
- Congenital infection is confirmed via PCR testing of neonatal saliva or urine within the first 3 weeks of life.
Strategies for CMV Prevention in Transplant Recipients
Transplant patients face high risk due to immunosuppressive regimens. Preventive strategies include:
1. Antiviral Prophylaxis
Prophylactic antiviral therapy is administered to all at-risk patients, regardless of viremia.
- Ganciclovir (IV) or Valganciclovir (oral) is the standard choice.
- Initiated immediately post-transplant and continued for 3–6 months.
- Valganciclovir: 900 mg daily (adjusted for renal function).
2. Preemptive Therapy
Targets early viral replication before symptoms appear.
- Patients are monitored weekly via CMV PCR or antigenemia assays.
- Therapy begins if viral load exceeds a defined threshold.
Preemptive therapy reduces drug exposure and toxicity, but requires strict monitoring compliance.
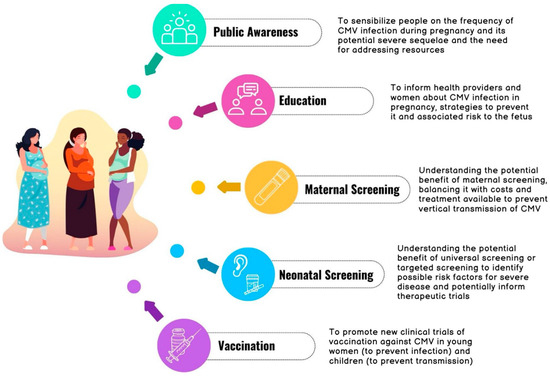
Prevention of Congenital Cytomegalovirus Infection
CMV is the leading cause of congenital viral infection, often resulting in hearing loss, microcephaly, and developmental delay.
Risk Reduction in Pregnancy
- Primary prevention via hand hygiene, especially after contact with young children’s saliva or urine.
- Seronegative pregnant women should avoid sharing food, utensils, or kissing on the mouth with toddlers.
- Routine CMV screening is not currently recommended for all pregnant women, but awareness campaigns are crucial.
Experimental Interventions
- CMV hyperimmune globulin (HIG) and antiviral therapy (e.g., valacyclovir) are under investigation for preventing fetal transmission.
Prevention in HIV-Infected Individuals
Patients with CD4+ counts <50 cells/μL are at high risk for CMV reactivation, particularly CMV retinitis.
ART as Primary Prevention
- Early and sustained antiretroviral therapy (ART) restores immune function and reduces CMV risk.
- Ophthalmologic exams every 3 months in patients with advanced disease.
- Routine antiviral prophylaxis for CMV is not recommended due to limited benefit and drug toxicity.
CMV Immunoglobulin Therapy: Adjunctive Role
CMV-specific immunoglobulin (CMV-IVIG) may be used in combination with antivirals in high-risk SOT patients or those with established CMV pneumonia post-HSCT.
- Reduces viral load and mitigates immune-mediated organ damage.
- Limited by cost and availability.
Infection Control Measures in Healthcare Settings
Hospitals and transplant centers must adhere to rigorous infection control protocols:
- Contact precautions for CMV-positive patients.
- Strict hand hygiene after handling secretions or body fluids.
- Use of leukoreduced and CMV-seronegative blood products in high-risk patients.
Emerging CMV Vaccines and Long-Term Prospects
Several CMV vaccine candidates are under development to prevent both congenital and post-transplant CMV disease.
Promising Approaches
- mRNA vaccines
- Recombinant viral vectors
- Subunit protein vaccines
These innovations aim to induce durable humoral and cellular immunity, particularly in women of childbearing age and transplant candidates.
Frequently Asked Questions
What is the most effective strategy to prevent CMV disease in transplant patients?
Universal antiviral prophylaxis using valganciclovir, especially in D+/R− settings, remains the most effective preventive approach.
Can CMV disease be completely prevented?
Not entirely, but the incidence and severity can be dramatically reduced through screening, prophylaxis, and immune restoration.
Is there a vaccine for CMV?
No licensed vaccine exists yet, but clinical trials for CMV vaccines, including mRNA-based candidates, are progressing.
How can congenital CMV be prevented?
Primary prevention through behavioral modifications in pregnancy is key. No approved antiviral or vaccine exists yet for routine use.
When is CMV immunoglobulin used?
It may be considered in high-risk transplant cases or CMV pneumonitis in HSCT recipients, usually in conjunction with antiviral therapy.
The prevention of cytomegalovirus disease is a multidimensional challenge requiring risk identification, virologic surveillance, and targeted prophylaxis. For transplant recipients, robust screening and timely antiviral administration form the cornerstone of prevention. In maternal and neonatal care, education and hygiene practices are essential to reducing congenital transmission. Among immunocompromised hosts, particularly HIV patients, immune restoration through ART remains paramount. As vaccine development advances, the long-term outlook for CMV control continues to improve.