Cidofovir, a nucleotide analog with broad-spectrum antiviral activity, is a potent agent used in the treatment of cytomegalovirus (CMV) retinitis and other DNA virus infections, particularly in immunocompromised patients. Despite its efficacy, cidofovir’s clinical utility is significantly limited by its high nephrotoxic potential. Without appropriate preventive strategies, the drug can cause irreversible kidney injury, necessitating early discontinuation and compromising therapeutic outcomes.
Understanding Cidofovir-Induced Nephrotoxicity
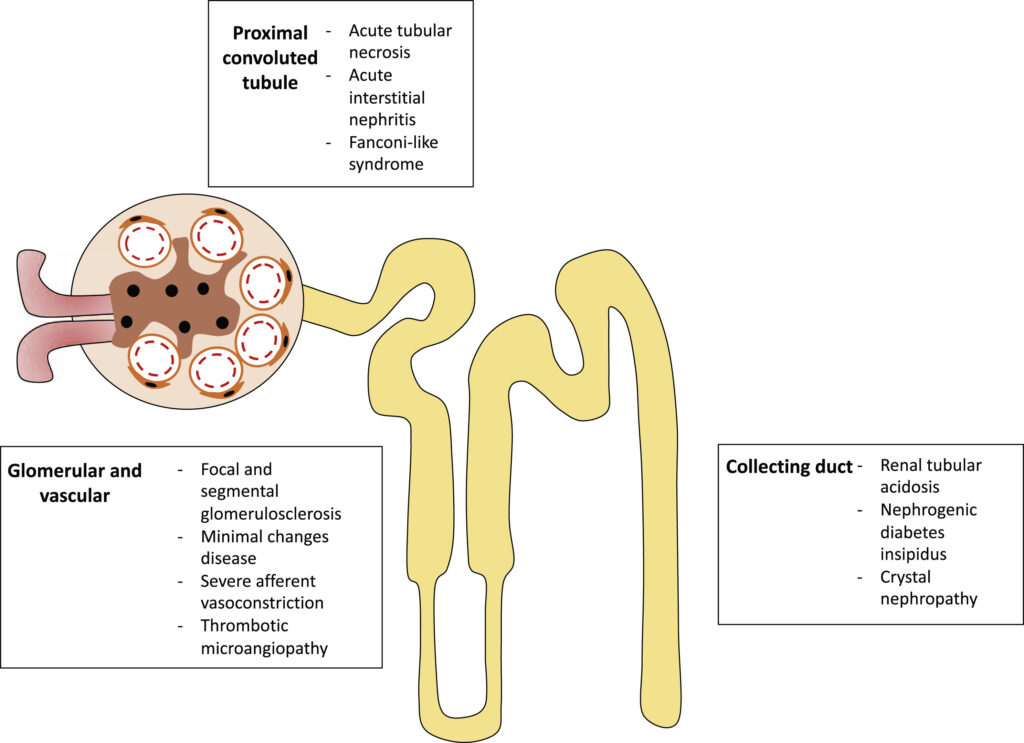
Cidofovir exerts its antiviral effect through inhibition of viral DNA polymerase. However, it is actively taken up by renal proximal tubular epithelial cells via the organic anion transporter 1 (OAT1), leading to intracellular accumulation and mitochondrial injury. This results in proximal tubular cell necrosis, impaired renal function, and in severe cases, acute kidney injury (AKI).
Key Mechanism of Nephrotoxicity
- Cellular uptake through OAT1 transporters
- Mitochondrial dysfunction and ATP depletion
- Proximal tubule necrosis
- Inflammatory cascade activation
High-Risk Factors for Cidofovir Nephrotoxicity
Several factors can amplify the risk of renal toxicity during cidofovir therapy.
| Risk Factor | Impact on Renal Function |
|---|---|
| Baseline renal impairment | Reduced clearance increases toxicity risk |
| Dehydration | Low intravascular volume heightens injury |
| Concurrent nephrotoxic drugs | Synergistic nephrotoxic potential |
| High cidofovir dosage | Dose-dependent tubular accumulation |
| Advanced age | Decline in renal reserve and GFR |
| Comorbidities (e.g., diabetes, hypertension) | Heightened susceptibility to renal injury |
Core Preventive Measures for Cidofovir-Induced Nephrotoxicity
1. Co-administration of Probenecid
Probenecid plays a critical role in minimizing cidofovir nephrotoxicity by competitively inhibiting OAT1 transporters in the renal tubules, thereby reducing cidofovir uptake and intracellular accumulation.
Probenecid Administration Protocol
- Dose: 2 g orally 3 hours before cidofovir infusion; followed by 1 g at 2 and 8 hours post-infusion
- Mechanism: Blocks tubular secretion of cidofovir via OAT1 inhibition
- Benefit: Substantially decreases renal cortical cidofovir concentration
2. Intravenous Saline Hydration
Adequate hydration prior to cidofovir infusion enhances urinary flow and reduces drug concentration in renal tubules, thus lowering contact time with tubular epithelial cells.
Hydration Protocol
- Normal Saline (0.9%): 1 L over 1–2 hours before cidofovir administration
- Additional 1 L post-infusion may be considered in high-risk cases
3. Avoidance of Concurrent Nephrotoxins
Cidofovir should not be administered alongside agents known to impair renal function. Drugs to avoid include:
- Aminoglycosides
- Amphotericin B
- NSAIDs
- IV contrast agents
Interruption or modification of such therapies is advisable when cidofovir is required.
4. Dose Adjustment Based on Renal Function
Cidofovir dosing should be guided by baseline serum creatinine and creatinine clearance (CrCl).
| CrCl (mL/min) | Recommended Action |
|---|---|
| >55 | Standard cidofovir dose (5 mg/kg) |
| 40–54 | Reduce dose or increase dosing interval |
| <40 | Cidofovir contraindicated |
Renal Monitoring and Surveillance Strategies
Baseline and Ongoing Assessments
- Serum Creatinine and BUN: Prior to each dose
- Urinalysis: Monitor for proteinuria or hematuria
- Electrolytes: Assess for Fanconi-like syndrome indicators (e.g., hypokalemia, hypophosphatemia)
- Creatinine Clearance: Calculate before each dose for dose adjustments
Discontinuation Criteria
Discontinue cidofovir if:
- Serum creatinine rises ≥0.4 mg/dL above baseline
- CrCl drops by ≥20% from baseline
- Proteinuria ≥2+ on dipstick persists
Complementary Protective Interventions
Antioxidants and Renal Support
Though not standard, some studies have evaluated adjunct use of antioxidants like N-acetylcysteine or ascorbic acid for renal protection, but robust clinical data are lacking. These are not routinely recommended in guidelines.
Therapeutic Drug Monitoring (TDM)
Although not widely available, TDM for cidofovir plasma levels could potentially guide individualized dosing in select high-risk populations, minimizing toxicity without sacrificing efficacy.
Summary of Best Practices
- Use probenecid in every patient to block tubular cidofovir uptake.
- Provide pre-infusion IV hydration with 1 L normal saline.
- Rigorously monitor renal function before every dose.
- Avoid concurrent nephrotoxic agents and adjust dosing for renal impairment.
- Educate patients on signs of renal dysfunction and ensure close follow-up.
Frequently Asked Questions
Why is cidofovir nephrotoxic?
Cidofovir accumulates in proximal renal tubules via OAT1, leading to cellular injury and necrosis, especially without prophylactic measures.
Can probenecid completely prevent nephrotoxicity?
While probenecid significantly reduces the risk, it does not eliminate it. Proper hydration and renal monitoring are also essential.
Is cidofovir safe in patients with mild renal dysfunction?
It may be used cautiously with dose adjustments, but is contraindicated if CrCl falls below 40 mL/min.
How long should hydration be continued?
Hydration is required only around each dose (pre- and possibly post-infusion), not on an ongoing daily basis.
Can cidofovir-induced nephrotoxicity be reversed?
If detected early and therapy is stopped promptly, partial to full recovery is possible. Delayed recognition may lead to permanent damage.
Preventing cidofovir-induced nephrotoxicity is crucial to maintaining the therapeutic efficacy of this antiviral agent while safeguarding renal function. A structured preventive approach—centered around probenecid use, IV hydration, renal function monitoring, and avoidance of nephrotoxic agents—must be strictly adhered to. Through diligent application of these strategies, we can optimize treatment outcomes and minimize the risk of kidney injury in patients requiring cidofovir therapy.