Cerebrovascular accidents (CVAs), commonly known as strokes, represent a leading cause of mortality and long-term disability worldwide. Effective prevention strategies are essential to reduce incidence and burden. This article presents a structured, evidence-based approach to preventing both ischemic and hemorrhagic strokes by addressing modifiable risk factors, implementing medical interventions, and promoting public health education.
Understanding Cerebrovascular Accidents: Classification and Causes
Types of Cerebrovascular Accidents
- Ischemic Stroke: Caused by an obstruction in cerebral blood vessels, typically from a thrombus or embolus.
- Hemorrhagic Stroke: Results from a ruptured blood vessel, leading to intracerebral or subarachnoid bleeding.
- Transient Ischemic Attack (TIA): Often called a “mini-stroke,” it is a warning sign of potential future strokes.
Primary Causes
- Atherosclerosis
- Hypertension
- Cardioembolic events (e.g., atrial fibrillation)
- Cerebral aneurysms
- Hypercoagulable states
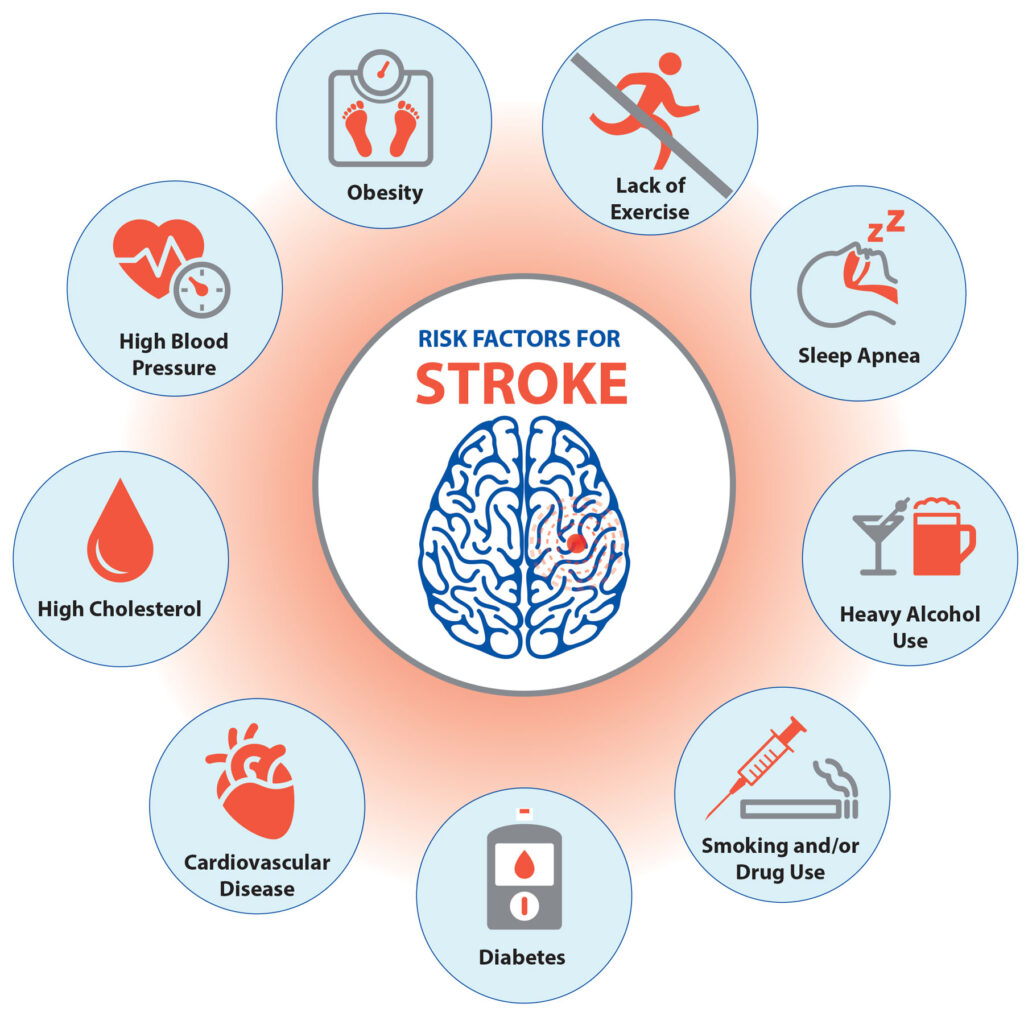
Risk Factor Identification and Management for Stroke Prevention
Non-Modifiable Risk Factors
- Age (greater risk over 55)
- Male gender
- Family history of stroke
- Genetic disorders (e.g., sickle cell disease)
Modifiable Risk Factors
| Risk Factor | Preventive Strategy |
|---|---|
| Hypertension | Blood pressure control (<130/80 mmHg) |
| Diabetes Mellitus | HbA1c < 7%, metformin, lifestyle change |
| Hyperlipidemia | Statins, diet modification |
| Smoking | Cessation programs, behavioral therapy |
| Obesity | Weight loss through diet/exercise |
| Physical Inactivity | ≥150 minutes of moderate activity/week |
| Excessive Alcohol | Limit to 1 drink/day (women), 2 (men) |
| Atrial Fibrillation | Anticoagulation (warfarin, DOACs) |
Medical Interventions for Stroke Prevention
Antiplatelet Therapy
- Aspirin (75–100 mg/day) is widely used in secondary prevention.
- Clopidogrel or combination therapy for aspirin intolerance or high-risk patients.
Anticoagulation for Cardioembolic Stroke
- Warfarin with INR monitoring (target 2.0–3.0)
- Direct Oral Anticoagulants (DOACs) such as apixaban, dabigatran, rivaroxaban
Blood Pressure Management
First-line agents include:
- ACE inhibitors (e.g., lisinopril)
- Calcium channel blockers (e.g., amlodipine)
- Thiazide diuretics
Lipid-Lowering Therapy
- Statins (e.g., atorvastatin, rosuvastatin) to reduce LDL cholesterol
- Consider ezetimibe or PCSK9 inhibitors for patients not reaching targets
Diabetes Management
- Metformin remains the first-line therapy
- SGLT2 inhibitors and GLP-1 receptor agonists provide cardiovascular protection
Lifestyle Modification as Primary Stroke Prevention
Nutritional Strategies
- DASH and Mediterranean diets lower stroke risk by reducing blood pressure and LDL.
- Emphasize: Whole grains, leafy greens, lean protein, nuts, and omega-3s.
Regular Physical Activity
- Aerobic and resistance training improve cardiovascular and cerebrovascular function.
- Target: Minimum 30 minutes/day, 5 days/week
Smoking Cessation
- Nicotine replacement, varenicline, or bupropion support abstinence.
- Counseling and support groups increase success rates.
Weight Reduction
- Sustained 5–10% weight loss significantly lowers stroke risk markers.
Diagnostic Monitoring and Preventive Screening
Routine Assessments
- Blood pressure: every 6–12 months
- Lipid profile: annually or semi-annually
- Blood glucose and HbA1c: every 3–6 months in diabetics
- ECG: to screen for arrhythmias such as atrial fibrillation
Imaging and Biomarker Evaluation
- Carotid Doppler ultrasound: detects arterial stenosis
- CT Angiography / MRI: identifies silent infarcts or aneurysms
- High-sensitivity CRP and homocysteine levels may indicate vascular inflammation
Interventional and Surgical Prevention Strategies
Carotid Artery Revascularization
- Carotid Endarterectomy (CEA): Indicated for patients with >70% stenosis and symptoms.
- Carotid Artery Stenting (CAS): For those unsuitable for surgery.
Aneurysm Management
- Surgical clipping or endovascular coiling to prevent rupture in unruptured aneurysms detected via screening.
Public Health and Community-Based Prevention
Awareness Campaigns
- Education on FAST symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call emergency) increases early detection and treatment.
Population-Level Interventions
- Salt reduction policies
- Tobacco taxation
- Hypertension screening clinics
Special Considerations in Stroke Prevention
Women
- Pregnancy and hormonal therapy increase risk—monitor blood pressure and coagulation markers.
- Preeclampsia history elevates future stroke risk.
Elderly Population
- Requires a careful balance between stroke prevention and bleeding risk.
- Comprehensive geriatric assessments guide therapy decisions.
Young Adults
- Focus on autoimmune causes, thrombophilias, and illicit drug use.
- Emphasize early intervention for modifiable risks.
Frequently Asked Questions
What is the most important factor in stroke prevention?
Controlling high blood pressure is the most impactful measure for both ischemic and hemorrhagic stroke prevention.
Is aspirin safe for everyone to prevent stroke?
Aspirin is typically reserved for high-risk individuals or those with prior cardiovascular events. Routine use in low-risk individuals may increase bleeding risk.
Can strokes be completely prevented?
While not all strokes are preventable, up to 80% of strokes can be avoided by modifying risk factors and adhering to preventive strategies.
How often should I be screened for stroke risk?
Annual evaluations are recommended for individuals over 40 or with known risk factors such as hypertension or diabetes.
Is there a difference in stroke prevention between ischemic and hemorrhagic types?
Yes. Ischemic stroke prevention focuses on antithrombotic therapy and vascular risk control, whereas hemorrhagic stroke emphasizes strict blood pressure regulation and avoidance of anticoagulants in non-indicated cases.