Cardiac transplant rejection remains a critical concern in post-operative care and long-term prognosis for heart transplant recipients. Timely prevention and control of immune-mediated graft injury are essential for preserving cardiac function, ensuring graft longevity, and improving patient survival. We present an in-depth exploration of preventive protocols, therapeutic advancements, and clinical monitoring essential to managing and reducing the risk of cardiac transplant rejection.
Understanding the Mechanisms of Cardiac Transplant Rejection
Immunological Basis
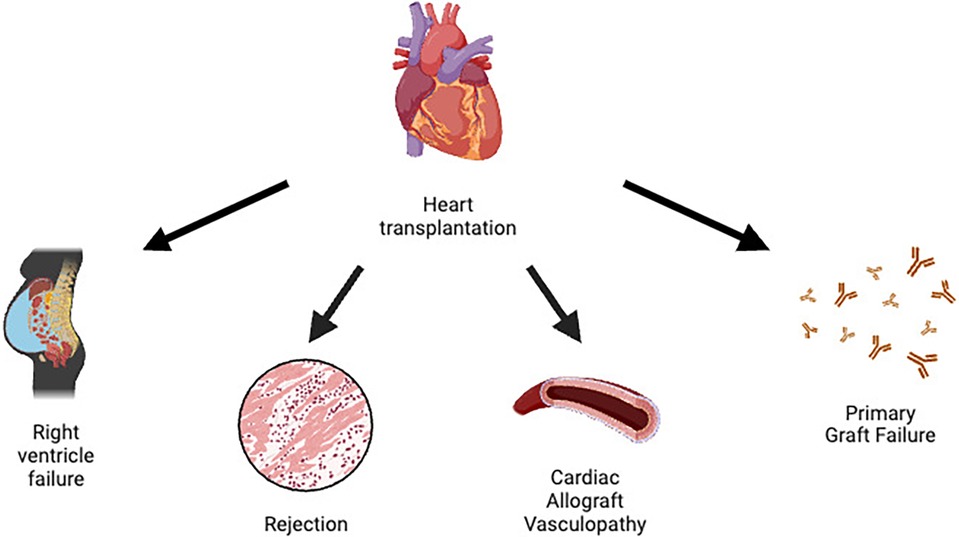
Rejection is an immunologic response where the recipient’s immune system recognizes the donor heart as foreign. The immune system, particularly T-cells and B-cells, initiates a cascade of reactions targeting the allograft, resulting in inflammation, vascular injury, and myocardial damage.
Types of Rejection
- Hyperacute Rejection: Occurs within minutes to hours due to pre-existing antibodies.
- Acute Cellular Rejection (ACR): Most common in the first year; T-cell mediated.
- Antibody-Mediated Rejection (AMR): Triggered by donor-specific antibodies (DSAs); associated with poor prognosis.
- Chronic Rejection/Cardiac Allograft Vasculopathy (CAV): Long-term immune injury causing vascular narrowing and ischemia.
Immunosuppressive Therapy: Cornerstone of Rejection Prevention
Induction Therapy
Administered perioperatively to reduce early rejection risk by depleting or modulating T-lymphocytes.
- Antithymocyte Globulin (ATG)
- Basiliximab (IL-2 receptor antagonist)
- Alemtuzumab (anti-CD52 monoclonal antibody)
Maintenance Immunosuppression
A lifelong regimen balancing rejection prevention with toxicity and infection risk.
Calcineurin Inhibitors (CNI)
- Tacrolimus: Preferred agent due to lower acute rejection rates.
- Cyclosporine: Alternative with distinct toxicity profile.
Antiproliferative Agents
- Mycophenolate Mofetil (MMF): Inhibits lymphocyte proliferation.
- Azathioprine: Less commonly used due to side-effect profile.
Corticosteroids
- Prednisone: Tapered over time but retained in high-risk patients.
mTOR Inhibitors
- Sirolimus or Everolimus: Useful in CAV prevention; may substitute or complement CNIs in selected cases.
Personalized Immunosuppression and Risk Stratification
Tailoring immunosuppressive therapy based on individual risk factors enhances efficacy and minimizes adverse effects.
Key Considerations
- Age, race, and prior sensitization
- HLA mismatch degree
- Presence of pre-formed or de novo DSAs
- Infection risk and renal function
Close collaboration with transplant immunologists ensures optimal therapeutic combinations.
Rigorous Monitoring to Detect and Prevent Rejection
Endomyocardial Biopsy (EMB)
- Gold standard for diagnosing acute rejection
- Performed at scheduled intervals post-transplant or when rejection is suspected
Non-Invasive Biomarkers and Imaging
- Gene expression profiling (e.g., AlloMap)
- Donor-derived cell-free DNA (dd-cfDNA)
- Echocardiography and Cardiac MRI to assess graft function
Routine surveillance facilitates early detection and prompt intervention.
Managing Antibody-Mediated Rejection (AMR)
AMR requires distinct therapeutic strategies:
- Plasmapheresis: Removes circulating DSAs
- Intravenous Immunoglobulin (IVIG): Modulates immune response
- Rituximab: Targets B-cell mediated antibody production
- Bortezomib or Eculizumab: Considered in refractory cases
Combination therapies are often employed to optimize outcomes in AMR management.
Prevention of Cardiac Allograft Vasculopathy (CAV)
CAV is a progressive form of chronic rejection involving diffuse intimal hyperplasia and luminal narrowing.
Prophylactic Measures
- Statins: Reduce inflammation and improve endothelial function
- mTOR inhibitors: Shown to inhibit smooth muscle proliferation
- Strict control of hypertension, diabetes, and hyperlipidemia
Annual coronary angiography or IVUS (intravascular ultrasound) aids in early detection and monitoring of CAV progression.
Infection Prophylaxis and Adherence
Immunosuppression increases infection susceptibility; hence, prophylactic regimens and patient compliance are crucial.
Standard Prophylaxis Includes
- CMV and Pneumocystis jirovecii pneumonia prophylaxis
- Fungal and bacterial infection surveillance
- Vaccination with inactivated agents
Patient education and close follow-up ensure regimen adherence and timely management of complications.
Lifestyle Modifications and Psychosocial Support
Long-term success post-transplant depends not only on medical therapy but also on holistic patient care.
Recommended Practices
- Regular physical activity under medical supervision
- Smoking cessation and alcohol moderation
- Balanced diet for cardiovascular and renal health
- Mental health support to address post-transplant stress and anxiety
Multidisciplinary transplant teams provide coordinated care across medical, psychological, and social domains.
Frequently Asked Questions
How is cardiac transplant rejection prevented?
Through lifelong immunosuppressive therapy, routine monitoring, and individualized risk-based care plans.
What is the most common form of cardiac transplant rejection?
Acute cellular rejection is the most frequently observed, especially within the first post-transplant year.
Are non-invasive tests reliable for rejection monitoring?
Yes, gene expression profiling and donor-derived cell-free DNA offer reliable, minimally invasive alternatives to biopsy in many cases.
Can lifestyle changes help prevent rejection?
While they don’t directly prevent immune rejection, healthy lifestyle choices enhance overall graft survival and reduce complications.
How long does a heart transplant last with proper prevention?
With diligent medical and lifestyle management, median survival exceeds 13 years, with many patients living two decades or more post-transplant.