Chemotherapy-induced thrombocytopenia (CIT) presents a significant clinical challenge in oncology, often necessitating dose reductions or delays in treatment. Proactive prevention strategies are essential to minimize patient risk, maintain therapeutic efficacy, and optimize clinical outcomes. This article presents an in-depth overview of the mechanisms, risk factors, and evidence-based interventions for preventing CIT.
Understanding Chemotherapy-Induced Thrombocytopenia
Pathophysiology and Clinical Impact
CIT results primarily from the myelosuppressive effects of chemotherapeutic agents on megakaryocyte progenitors in the bone marrow. This reduction in platelet production may lead to increased bleeding risk, treatment interruptions, and compromised therapeutic efficacy.
Common Culprit Agents
Chemotherapeutic drugs frequently associated with thrombocytopenia include:
- Carboplatin
- Gemcitabine
- Temozolomide
- Topotecan
Risk correlates with cumulative dose intensity and patient-specific factors such as baseline marrow reserve and coexisting conditions.
Identifying High-Risk Populations
Proactive prevention begins with risk stratification. Patients at increased risk for CIT include:
- Age > 65 years
- Preexisting cytopenias
- Prior exposure to intensive chemotherapy
- Liver dysfunction
- Concurrent use of myelosuppressive agents
Utilizing predictive models, such as the Thrombocytopenia Risk Assessment Tool, enables clinicians to implement tailored prophylactic strategies.
Pharmacologic Prevention Strategies
Thrombopoietin Receptor Agonists (TPO-RAs)
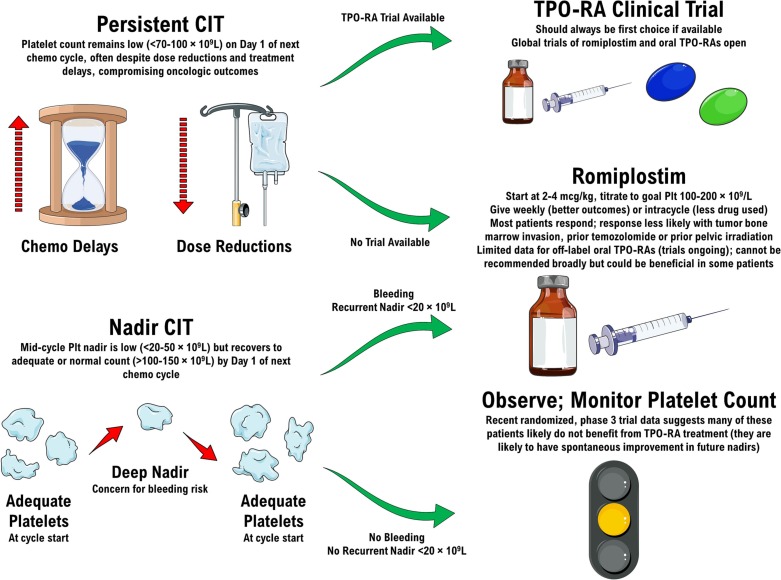
TPO-RAs stimulate platelet production and have demonstrated efficacy in reducing the incidence and severity of CIT.
Romiplostim
- Administered subcutaneously
- Dosing based on platelet count trends
- Shown to decrease chemotherapy dose delays
Eltrombopag
- Oral administration
- Well-tolerated with minimal hepatotoxicity
- Requires liver function monitoring during use
Interleukin-11 (Oprelvekin)
- Promotes megakaryocyte maturation
- Limited by cardiovascular side effects and fluid retention
- Reserved for selected patients unresponsive to TPO-RAs
Non-Pharmacologic and Supportive Measures
Chemotherapy Regimen Modifications
Adjusting the dose or frequency of thrombocytopenia-inducing agents may prevent severe platelet depletion. Strategies include:
- Dose reduction without compromising efficacy
- Prolonging treatment intervals
- Utilizing combination regimens with lower hematologic toxicity
Platelet Transfusions
Although primarily therapeutic, transfusions serve a prophylactic role in high-risk scenarios such as:
- Platelet counts < 10,000/µL
- Anticipated invasive procedures
- Severe mucositis or bleeding diathesis
Frequent monitoring is essential to guide transfusion thresholds.
Integrating Predictive Analytics and Personalized Care
Emerging technologies in artificial intelligence and machine learning are enhancing the prediction and prevention of CIT. Algorithms analyzing patient-specific data—such as genomics, prior treatment response, and real-time blood counts—facilitate individualized prophylactic interventions.
Clinical Guidelines and Evidence-Based Protocols
Organizations such as the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) recommend the following:
- Routine platelet monitoring during chemotherapy
- Consideration of TPO-RAs in recurrent CIT
- Use of risk-adapted chemotherapy planning
Clinical decision-making should be guided by the balance between thrombocytopenia risk and therapeutic goals.
Future Directions in CIT Prevention
Novel Agents in Development
- Avatrombopag and Lusutrombopag, originally approved for thrombocytopenia in liver disease, are under investigation for CIT prevention.
- Gene therapy and bone marrow microenvironment modulation may offer long-term solutions.
Integration with Immunotherapy
With the rise of immunotherapy and targeted treatments, synergistic strategies are needed to mitigate hematologic toxicity while maintaining immune modulation.
Preventing chemotherapy-induced thrombocytopenia is critical to maintaining treatment intensity, enhancing patient outcomes, and reducing complications. A multi-pronged approach—including pharmacologic agents like TPO-RAs, personalized care plans, and adherence to clinical guidelines—offers the best defense against CIT. Continued research and integration of predictive analytics will further refine prevention strategies, paving the way for safer, more effective cancer therapy.