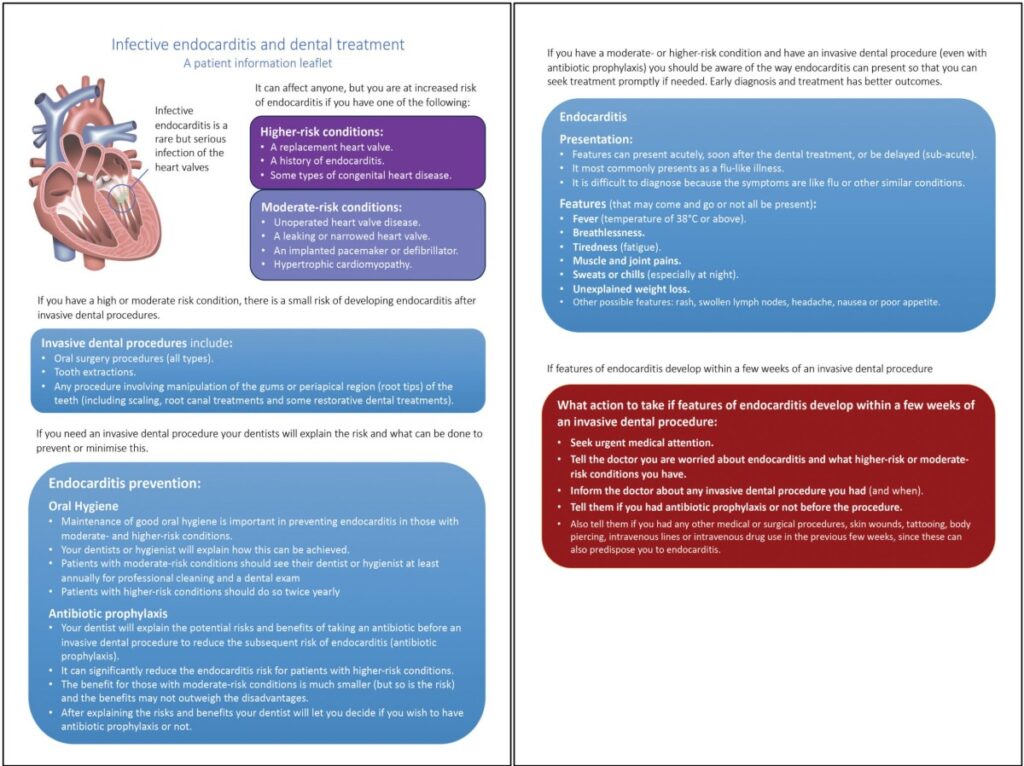
Bacterial endocarditis, also known as infective endocarditis (IE), is a serious and potentially life-threatening infection of the heart valves or endocardium. Prevention of bacterial endocarditis focuses on identifying high-risk individuals, maintaining optimal oral health, and implementing targeted antibiotic prophylaxis before specific medical or dental procedures.
Understanding Bacterial Endocarditis and Its Pathogenesis
Bacterial endocarditis results from microbial infection—typically from Streptococcus, Staphylococcus, or Enterococcus species—entering the bloodstream and colonizing damaged endocardial surfaces. The formation of vegetations can cause valve destruction, embolic events, and systemic complications.
Key Risk Factors
- Prosthetic heart valves (mechanical or bioprosthetic)
- Previous history of infective endocarditis
- Certain congenital heart diseases (CHDs)
- Cardiac transplant recipients with valve regurgitation
- Intravenous drug use
- Poor dental hygiene and invasive procedures
Antibiotic Prophylaxis for High-Risk Patients
Antibiotic prophylaxis is reserved for those at highest risk of developing IE. According to the American Heart Association (AHA) and European Society of Cardiology (ESC), prophylaxis is warranted only in selected cases.
Indications for Antibiotic Prophylaxis
- Dental procedures involving manipulation of gingival tissue or perforation of the oral mucosa
- Respiratory tract procedures involving incision or biopsy of mucosa
- Infected skin or musculoskeletal tissue interventions
Prophylaxis is not recommended for gastrointestinal or genitourinary tract procedures unless infection is present.
Recommended Regimens
| Patient Group | Standard Oral Regimen | Penicillin-Allergic Regimen |
|---|---|---|
| Adults | Amoxicillin 2g, 1 hour before | Clindamycin 600mg, 1 hour before |
| Children | Amoxicillin 50 mg/kg | Clindamycin 20 mg/kg |
Single-dose regimens are effective and reduce unnecessary antibiotic use.
Preventive Oral Hygiene Practices
Maintaining oral hygiene is a cornerstone in the long-term prevention of bacterial endocarditis, especially for individuals with cardiac risk factors.
Recommended Oral Care Guidelines
- Brush teeth at least twice daily with fluoride toothpaste
- Floss daily to prevent gingival inflammation and bacteremia
- Routine professional dental cleanings every 6 months
- Prompt management of dental infections or caries
- Avoid oral piercings or self-treatment of gum issues
Educating patients on the oral-systemic connection is vital for adherence.
Procedural Considerations and Risk Assessment
Not all invasive procedures require antibiotic prophylaxis. A thorough risk assessment should guide clinical decisions.
Cardiac Risk Categories
| Risk Level | Conditions |
|---|---|
| High Risk | Prosthetic valves, prior IE, unrepaired cyanotic CHD |
| Moderate Risk | Acquired valve disease, hypertrophic cardiomyopathy |
| Low Risk | Pacemakers, coronary artery bypass grafts |
Only high-risk individuals require prophylactic antibiotics for qualifying procedures.
Avoiding Unnecessary Antibiotic Use
Overprescribing antibiotics can lead to resistance, adverse reactions, and increased healthcare costs. As such, strict adherence to updated guidelines is crucial.
Principles of Rational Antibiotic Use
- Prescribe only when benefit clearly outweighs risk
- Use narrow-spectrum agents appropriate to the infection risk
- Educate patients on why prophylaxis may not be necessary for most
Clinicians should document rationale and educate patients clearly to promote trust and understanding.
Special Populations and Considerations
Pediatric Patients
- Children with congenital heart defects must be assessed based on defect type and surgical repair history
- Dosage adjustment by weight is mandatory for pediatric antibiotic regimens
Immunocompromised Patients
- While immunosuppression increases infection risk, IE prophylaxis is not routinely indicated without cardiac risk factors
Pregnant Patients
- Penicillin and clindamycin are generally safe in pregnancy for prophylaxis
- Care must be taken with antibiotic choice in allergic individuals
Emerging Trends in Endocarditis Prevention
Novel Preventive Measures
- Research into antibiofilm agents to prevent microbial adhesion on heart valves
- Development of vaccines targeting IE-associated pathogens
- Use of point-of-care diagnostics to rapidly assess bacteremia risk before procedures
Integration of Digital Health Tools
- Electronic dental records with alerts for cardiac risk
- Mobile apps for medication reminders and oral hygiene tracking
- Telemedicine follow-ups for at-risk patients post-procedures
The prevention of bacterial endocarditis hinges on meticulous identification of at-risk individuals, judicious use of antibiotic prophylaxis, and unwavering commitment to oral hygiene. By aligning clinical practice with evidence-based guidelines and empowering patients through education, we can substantially reduce the incidence and consequences of this life-threatening condition.