Re-bleeding from an acute gastrointestinal ulcer is a serious complication associated with significant morbidity and mortality. Despite advances in therapeutic endoscopy and pharmacologic interventions, recurrence remains a risk, particularly within the first 72 hours post-bleed. Effective prevention requires a multifaceted approach combining endoscopic management, pharmacotherapy, eradication of underlying causes, and long-term risk reduction strategies.
Understanding Acute Gastrointestinal Ulcer Bleeding and Re-Bleed Risk
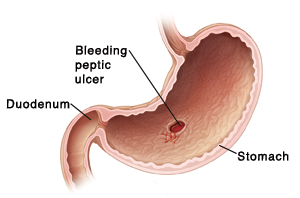
Acute gastrointestinal ulcers, whether gastric or duodenal, may bleed due to mucosal erosion involving submucosal vessels. Once bleeding occurs, the likelihood of re-bleed—especially in high-risk patients—can be as high as 20%.
Risk factors for ulcer re-bleeding include:
- Active spurting or oozing on endoscopy (Forrest Ia/Ib)
- Visible vessels or adherent clots (Forrest IIa/IIb)
- NSAID or antiplatelet use
- Helicobacter pylori infection
- History of previous GI bleeding
- Advanced age and comorbidities (e.g., liver cirrhosis, renal failure)
Early Endoscopic Hemostasis: Cornerstone of Re-Bleed Prevention
Endoscopy performed within 24 hours of presentation is essential in both diagnosing and controlling the source of bleeding.
Endoscopic Hemostatic Techniques
- Injection therapy: Epinephrine followed by a second modality
- Thermal coagulation: Bipolar or heater probe
- Mechanical therapy: Hemoclips for high-risk stigmata
- Combination therapy: Proven superior for reducing re-bleeding
Post-endoscopic risk stratification guides further medical therapy and monitoring intensity.
High-Dose Proton Pump Inhibitor (PPI) Therapy: Medical Mainstay
Proton pump inhibitors are critical in reducing gastric acidity, promoting clot stability, and preventing re-bleeding.
Recommended PPI Protocol Post-Endoscopy
- Initial 72 hours: Intravenous omeprazole or pantoprazole 80 mg bolus, then 8 mg/hour continuous infusion
- Subsequent therapy: High-dose oral PPI (e.g., omeprazole 40 mg twice daily) for 4–8 weeks
Clinical trials confirm that high-dose PPIs significantly reduce re-bleeding, surgical intervention, and mortality rates.
Eradication of Helicobacter pylori: Essential for Ulcer Healing and Recurrence Prevention
H. pylori is implicated in over 90% of duodenal ulcers and a large proportion of gastric ulcers.
Eradication Strategy
- Confirm presence via urea breath test, stool antigen, or biopsy
- Initiate triple therapy: PPI + amoxicillin + clarithromycin for 14 days
- Confirm eradication after 4–6 weeks post-treatment
Failure to eliminate H. pylori increases the risk of recurrent bleeding and chronic ulceration.
NSAID and Antiplatelet Management: Addressing the Root Cause
NSAIDs and antiplatelets are frequent culprits in ulcer development and re-bleeding.
Strategies for At-Risk Patients
- Discontinue NSAIDs whenever possible
- If essential, use COX-2 inhibitors with concurrent PPI
- Aspirin for cardiovascular prophylaxis should be restarted cautiously (usually within 3–5 days post-bleed under PPI cover)
- Consider misoprostol as an alternative mucosal protective agent
Decision-making must balance GI bleeding risk with thrombotic risk.
Long-Term Maintenance Therapy in High-Risk Patients
Patients with a history of ulcer bleeding and persistent risk factors (e.g., continued antithrombotic therapy, elderly) may require extended prophylaxis.
- Long-term once-daily PPI therapy
- Regular surveillance endoscopy for recurrent symptoms or alarm signs
- Iron supplementation if anemia persists post-bleed
Gastroenterology follow-up is essential for ongoing assessment.
Lifestyle Modifications to Support Ulcer Healing and Prevent Re-Bleed
While not substitutes for medical therapy, certain lifestyle interventions support gastric mucosal integrity and reduce ulcer recurrence.
Key Recommendations
- Avoid tobacco and alcohol, both of which impair mucosal defense
- Eat smaller, more frequent meals to avoid gastric overdistension
- Avoid late-night eating and known irritants (spicy food, caffeine)
- Maintain optimal hydration and stress management
Patient education plays a critical role in ensuring adherence to both medical and behavioral regimens.
When to Re-Evaluate or Escalate Care
Prompt reassessment is critical when patients exhibit:
- Recurrent hematemesis or melena
- Hemodynamic instability after initial stabilization
- Drop in hemoglobin despite transfusion
These signs warrant repeat endoscopy, consideration of angiographic embolization, or surgical intervention in refractory cases.
Preventing acute gastrointestinal ulcer re-bleed requires timely intervention, meticulous pharmacological management, eradication of causative agents, and long-term follow-up. Through evidence-based strategies and comprehensive patient care, we can significantly reduce recurrence and enhance clinical outcomes in high-risk populations.

