Extracorporeal clotting during hemodialysis is a critical complication that compromises treatment efficacy, patient safety, and equipment longevity. This phenomenon occurs when blood components activate coagulation pathways while in contact with the dialysis circuit, leading to clot formation outside the body. Proper prevention and management of this condition require a comprehensive, multidisciplinary approach involving pharmacologic, mechanical, and procedural interventions.
Understanding the Mechanism of Extracorporeal Clotting
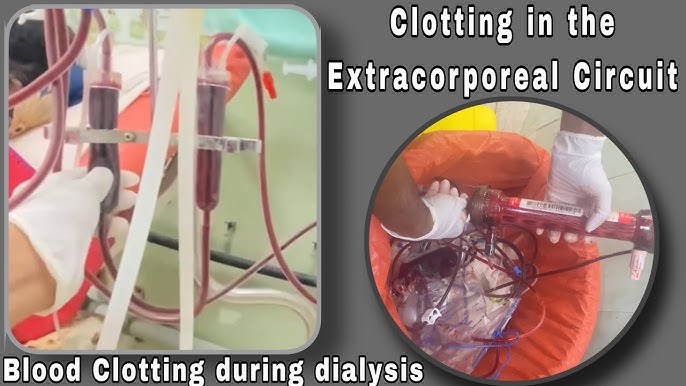
Clot formation during hemodialysis results from the exposure of blood to artificial surfaces, leading to platelet activation, fibrin deposition, and thrombus development. The clotting cascade is initiated by:
- Contact with non-endothelial surfaces
- Turbulent or slowed blood flow
- Insufficient anticoagulation
- Air interface exposure within the circuit
Once initiated, clotting can escalate rapidly, impairing circuit function and requiring premature termination of the dialysis session.
Anticoagulation Protocols for Clot Prevention
1. Systemic Heparinization
Heparin remains the gold standard for anticoagulation in hemodialysis. Administered as a bolus or continuous infusion, unfractionated heparin (UFH) prevents fibrin formation by enhancing antithrombin III activity.
Advantages:
- Rapid onset of action
- Easy reversibility with protamine sulfate
- Effective in most patients
Monitoring Parameters:
- Activated clotting time (ACT)
- Partial thromboplastin time (PTT)
- Clinical signs of bleeding or clotting
2. Low Molecular Weight Heparin (LMWH)
LMWHs such as enoxaparin offer predictable pharmacokinetics and longer half-life, making them suitable for single-bolus administration at the start of dialysis.
Caution: Not ideal for patients at high bleeding risk or with limited renal clearance.
3. Regional Citrate Anticoagulation (RCA)
RCA is preferred in patients with high bleeding risk. Citrate chelates ionized calcium, a key cofactor in the clotting cascade, thereby preventing coagulation within the circuit. Calcium is then infused systemically to maintain physiologic levels.
4. Heparin-Free Dialysis
Indicated in cases of active bleeding, heparin-induced thrombocytopenia (HIT), or severe coagulopathy. Techniques to mitigate clotting without anticoagulants include:
- Saline flushes (100 mL every 15–30 minutes)
- High blood flow rates
- Use of coated dialyzers
Circuit Design and Blood Flow Optimization
Mechanical adjustments can reduce shear stress and stagnation zones that promote clotting:
- Use of biocompatible dialyzers: Surface-modified membranes reduce platelet adhesion.
- Shorter tubing length: Minimizes surface area for clot activation.
- Maintaining optimal blood flow rate (Qb): 300–500 mL/min is typically effective.
- Appropriate dialysate flow (Qd): Typically 500–800 mL/min to ensure efficient clearance and temperature control.
- Minimized air-blood contact: Ensures low turbulence and reduced activation of clotting factors.
Monitoring for Early Detection of Clotting
Continuous surveillance during hemodialysis allows for early identification and intervention:
| Parameter | Normal Range | Clotting Indicator |
|---|---|---|
| Arterial Pressure | -100 to -250 mmHg | Unexpected increase (resistance) |
| Venous Pressure | 100 to 200 mmHg | Steady rise (obstruction) |
| Transmembrane Pressure | Varies by patient | Sudden increase |
| Visual Inspection | Clear blood chamber | Fibrin strands or dark discoloration |
Prompt action upon deviation includes circuit flushing, anticoagulation adjustment, or circuit replacement.
Special Considerations in High-Risk Populations
1. Patients with Bleeding Risk
- Use RCA or heparin-free strategies
- Monitor ionized calcium and total calcium
- Avoid prolonged treatments that raise clotting likelihood
2. Patients with Heparin-Induced Thrombocytopenia (HIT)
- Discontinue all forms of heparin
- Use direct thrombin inhibitors (e.g., argatroban) as alternative
- Monitor platelet counts and coagulation markers closely
3. Pediatric and Neonatal Patients
- Require lower blood flow rates and circuit volumes
- Anticoagulant dosing must be weight-adjusted
- Extra care in monitoring for clotting and circuit kinks
Protocol-Based Approach to Clot Prevention
Developing standardized institutional protocols ensures consistency and safety. A comprehensive approach includes:
- Pre-dialysis evaluation: Coagulation profile, anticoagulant contraindications
- Anticoagulation order set: Based on patient-specific risk stratification
- Intra-dialysis monitoring: Real-time pressure tracking and visual assessments
- Post-dialysis documentation: Anticoagulation efficacy and circuit integrity
Emerging Technologies in Hemodialysis Anticoagulation
Innovative strategies under investigation to further reduce clotting risks include:
- Surface-modified circuits with heparin coatings
- Nanotechnology-enhanced membranes
- Bioengineered surfaces mimicking endothelium
- Closed-loop anticoagulation systems with AI-based feedback
Such advancements hold promise in improving safety and cost-effectiveness, especially for chronic dialysis populations.
Preventing extracorporeal clotting during hemodialysis is a multidimensional challenge requiring optimized anticoagulation, vigilant circuit design, and proactive monitoring. Individualized protocols based on patient risk factors, coupled with emerging innovations in device technology, enable safer and more effective dialysis outcomes. Vigilance, adaptation, and protocol adherence are essential pillars in the sustained success of extracorporeal clot prevention.