Methylmalonic acidemia (MMA) is a rare but serious genetic metabolic disorder that affects the body’s ability to break down certain fats and proteins. This condition is caused by a deficiency of the enzyme methylmalonyl-CoA mutase, which is involved in metabolizing specific amino acids and lipids. As a result, toxic levels of methylmalonic acid build up in the body, leading to a variety of life-threatening complications, particularly affecting the nervous system, kidneys, and other vital organs.
The severity of MMA can range from mild to severe, and its impact on the individual can vary. In newborns and infants, MMA can cause acute metabolic crises, developmental delays, and long-term neurological impairments. Early diagnosis and intervention are crucial for improving the prognosis of affected individuals.
Prenatal care for expectant mothers carrying a fetus with MMA requires careful monitoring and management to reduce the risks associated with this disorder. With the advancement of prenatal testing and treatment options, it is possible to manage the effects of MMA more effectively, ensuring better health outcomes for both the mother and the baby.
Causes and Inheritance of Methylmalonic Acidemia
MMA is inherited in an autosomal recessive pattern, meaning that both parents must carry a copy of the mutated gene for a child to inherit the condition. The gene mutations that cause MMA affect the MUT gene, which is responsible for producing the enzyme needed for proper metabolism of methylmalonyl-CoA.
When both parents are carriers, there is a 25% chance in each pregnancy that the child will inherit two copies of the mutated gene, resulting in MMA. Prenatal genetic screening and diagnostic testing are essential tools for identifying at-risk pregnancies, enabling early intervention to manage the disorder.
Key Causes of MMA:
- Deficiency of methylmalonyl-CoA mutase enzyme
- Mutations in the MUT gene responsible for enzyme production
- Inborn errors of metabolism related to metabolic pathways
Prenatal Diagnosis of Methylmalonic Acidemia
The early identification of MMA in a fetus is critical for effective prenatal management. Several diagnostic tests can be performed during pregnancy to assess the risk of MMA and other metabolic disorders.
1. Carrier Screening for Parents
- Carrier screening is offered to couples who may be at risk of passing on genetic disorders like MMA. This involves blood tests that check for the presence of the MMA gene mutation in both parents. If both parents are carriers of MMA, there is a 25% chance that their child will be born with the condition.
2. Non-invasive Prenatal Testing (NIPT)
- Non-invasive prenatal testing can screen for genetic conditions such as MMA by analyzing small fragments of fetal DNA present in the mother’s blood. NIPT has become an essential tool for identifying the risk of MMA and other genetic disorders without invasive procedures.
3. Amniocentesis and Chorionic Villus Sampling (CVS)
- Amniocentesis and chorionic villus sampling (CVS) are invasive diagnostic tests that can confirm the presence of MMA by testing the amniotic fluid or tissue from the placenta. These tests can be performed later in the pregnancy, typically between the 15th and 20th week, to analyze fetal DNA and identify genetic mutations.
4. Metabolic Screening via Blood Tests
- Prenatal metabolic screening can help detect elevated levels of metabolites like methylmalonic acid, which may indicate the presence of MMA. Elevated methylmalonic acid levels in maternal blood can be a warning sign of the disorder.
Prenatal Treatment and Management of MMA
Managing MMA during pregnancy requires a multi-disciplinary approach involving genetic counseling, metabolic specialists, obstetricians, and neonatologists. Prenatal interventions aim to reduce the severity of the disorder in the fetus and ensure the best possible outcomes.
1. Maternal Dietary Management
- One of the most critical aspects of managing MMA during pregnancy is dietary modification. Expectant mothers who carry a fetus with MMA may be instructed to follow a strict low-protein diet to reduce the intake of amino acids that could lead to the buildup of toxic metabolites.
- Vitamin B12 supplementation may also be recommended, as methylmalonic acidemia can be linked to deficiencies in vitamin B12, which is necessary for proper metabolism.
2. Fetal Monitoring
- Frequent fetal monitoring through ultrasound and biophysical profiles is essential to track the health and development of the fetus. This allows healthcare providers to identify any complications early, ensuring timely interventions.
- Regular monitoring of fetal growth and amniotic fluid levels can also help detect signs of metabolic imbalance that might indicate MMA.
3. Prenatal Enzyme Therapy
- Emerging treatments such as enzyme replacement therapy (ERT) may be an option for some pregnant women with MMA. ERT involves administering synthetic or bioengineered enzymes to replace the deficient enzyme, reducing the buildup of toxic substances. While research is ongoing, early results have shown promise in improving metabolic control in MMA patients.
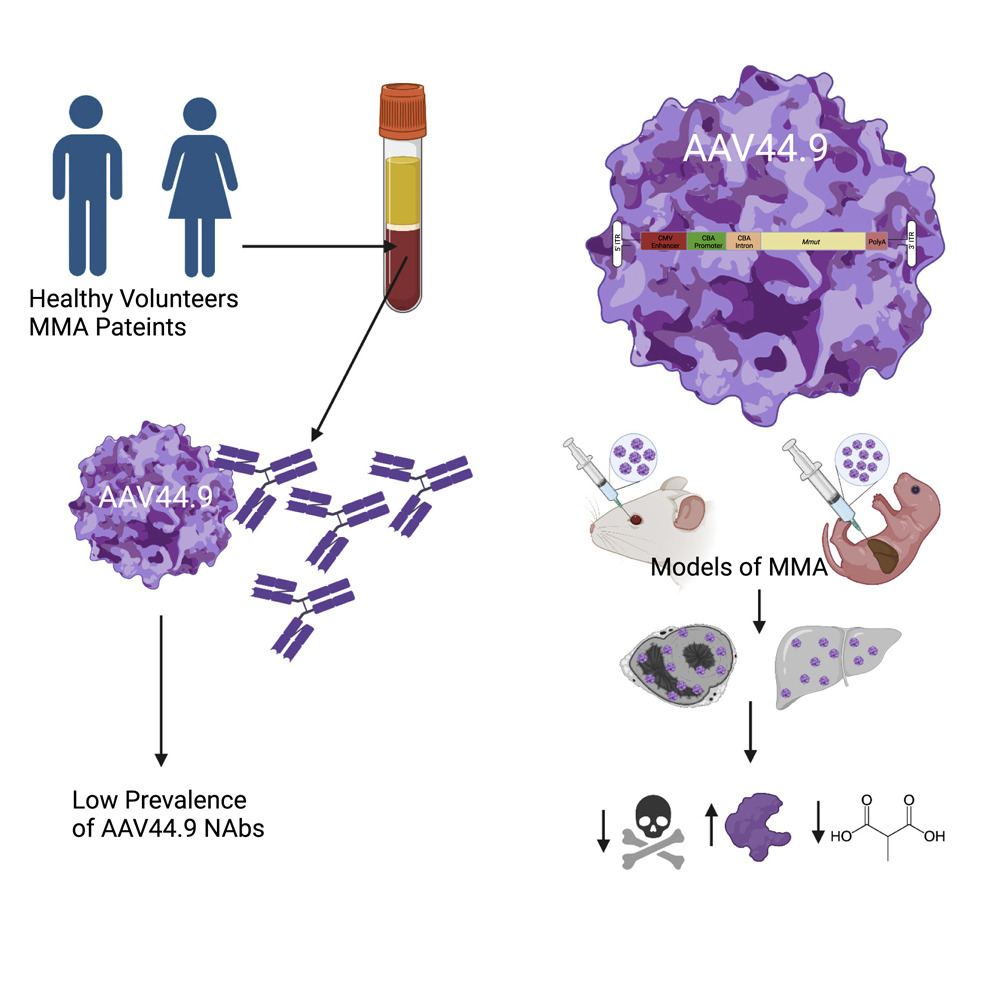
4. Gene Therapy and Experimental Interventions
- Gene therapy is a promising area of research for the prenatal treatment of MMA. Although it is still in the experimental stages, gene therapy aims to introduce a healthy copy of the MUT gene into the fetus’s cells, potentially correcting the underlying genetic defect. This intervention, however, is not yet widely available and requires further studies to determine its efficacy.
5. Early Delivery and Neonatal Care
- In cases where MMA is detected late in pregnancy, early delivery may be considered if the fetus is showing signs of metabolic distress. Postpartum, babies born with MMA require immediate neonatal intensive care, which may include metabolic stabilization and enzyme replacement therapies.
Postpartum Care and Long-Term Management of MMA
Once the baby is born, the management of MMA continues with specialized care and ongoing monitoring to prevent metabolic crises and long-term complications.
1. Enzyme Replacement Therapy (ERT)
- Enzyme replacement therapy (ERT) is often initiated at birth for infants diagnosed with MMA. This treatment helps reduce the accumulation of methylmalonic acid in the body, improving overall metabolic stability and reducing the risk of developmental delays or neurological impairment.
2. Dietary Modifications
- Infants diagnosed with MMA will require strict dietary management to ensure they do not ingest excessive levels of amino acids or lipids. This often involves working with a metabolic nutritionist to create a personalized diet plan that supports growth while managing the disease.
3. Monitoring Growth and Development
- Regular monitoring of the infant’s growth, neurological development, and metabolic status is crucial in the first few years of life. Early intervention can help manage developmental delays and ensure that the child reaches critical milestones in their early life.
Prenatal treatment of methylmalonic acidemia presents significant challenges but also offers hope through early diagnosis and innovative treatment strategies. With advances in genetic testing, prenatal care, and potential therapies, expectant mothers can manage the risks associated with MMA and provide their children with the best possible chance for a healthy life. Early intervention and close monitoring are essential in minimizing the impact of this metabolic disorder, ensuring both maternal and fetal well-being throughout pregnancy and beyond.