Postsurgical vaginal cuff anaerobic infections represent a significant complication following gynecologic surgeries, especially total hysterectomy. These infections are primarily polymicrobial, with anaerobic bacteria such as Bacteroides fragilis, Peptostreptococcus, and Prevotella species playing a prominent role. Prompt recognition and aggressive management are imperative to prevent morbidity and long-term sequelae, including abscess formation, pelvic cellulitis, and peritonitis.
Etiology and Pathogenesis
Anaerobic Microflora of the Female Genital Tract
The lower genital tract harbors a diverse bacterial flora, including anaerobes that can ascend postoperatively. Disruption of the vaginal mucosa and surgical manipulation during hysterectomy or colpotomy provide a pathway for these organisms to infect the vaginal cuff and surrounding pelvic tissues.
Common Anaerobic Pathogens Involved
- Bacteroides fragilis
- Peptostreptococcus spp.
- Prevotella spp.
- Clostridium spp.
- Fusobacterium spp.
These organisms thrive in oxygen-deprived environments and are particularly virulent due to their ability to produce tissue-destroying enzymes and evade host immune responses.
Risk Factors for Vaginal Cuff Anaerobic Infections
- Total abdominal or laparoscopic hysterectomy
- Poor surgical technique or inadequate cuff closure
- Use of electrocautery at the cuff margin
- Pre-existing vaginal infections or bacterial vaginosis
- Obesity, diabetes, or immunocompromised states
- Smoking and poor wound healing capacity
- Use of non-absorbable suture material
- Early resumption of vaginal intercourse post-surgery
Each of these factors either introduces bacteria into the operative field or impairs the body’s ability to clear pathogens postoperatively.
Clinical Presentation and Symptoms
Patients typically present within 5 to 14 days postoperatively. Symptoms can be acute or insidious and may include:
- Pelvic pain and pressure
- Malodorous or purulent vaginal discharge
- Fever (>38°C) and chills
- Vaginal bleeding or spotting
- Dyspareunia (painful intercourse)
- Pelvic tenderness on examination
- Leukocytosis on complete blood count (CBC)
In more severe cases, abscess formation, septicemia, and pelvic peritonitis may occur, necessitating urgent intervention.
Diagnostic Evaluation
Physical Examination
A speculum and bimanual examination are essential. Findings may include cuff induration, erythema, purulent discharge, and cervical motion tenderness. In severe cases, a fluctuant mass indicating abscess may be palpable.
Laboratory Testing
- CBC: Elevated white blood cell count with left shift
- CRP/ESR: Markedly elevated in systemic inflammatory response
- Vaginal culture: To guide targeted antimicrobial therapy
- Blood cultures: For systemic infections or suspected bacteremia
Imaging Modalities
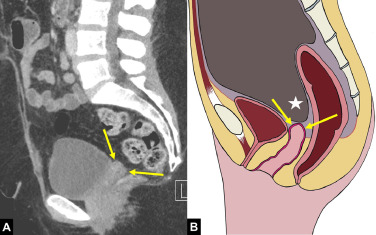
Transvaginal Ultrasonography
- First-line imaging to assess for fluid collections or abscess
Pelvic CT or MRI
- For deeper evaluation of complex cases, suspected pelvic abscesses, or when ultrasound is inconclusive
Management and Treatment Strategies
Empirical Antimicrobial Therapy
Initiation of broad-spectrum antibiotics covering anaerobes is critical. Preferred regimens include:
- IV Clindamycin + Gentamicin
- IV Ampicillin/Sulbactam
- IV Piperacillin/Tazobactam
- IV Metronidazole + Ceftriaxone
Duration typically ranges from 7–14 days, depending on clinical response. Transition to oral therapy may be considered upon improvement.
Drainage of Abscesses
If imaging reveals a localized abscess, drainage is often required:
- Percutaneous or transvaginal drainage under ultrasound or CT guidance
- Surgical drainage if percutaneous options fail or patient deteriorates
Surgical Re-intervention
In rare cases, especially when the vaginal cuff has dehisced or there is extensive infection:
- Exploratory laparoscopy or laparotomy may be warranted
- Cuff re-suturing or debridement may be necessary
Preventive Measures and Prophylaxis
Intraoperative Precautions
- Use of absorbable monofilament sutures
- Adequate hemostasis
- Minimizing use of electrosurgical energy on vaginal cuff
- Thorough irrigation and removal of necrotic tissue
Preoperative Preparation
- Treatment of existing bacterial vaginosis or vaginitis
- Preoperative vaginal cleansing with antiseptic solution
- Antibiotic prophylaxis (e.g., cefazolin + metronidazole) before incision
Postoperative Recommendations
- Avoidance of vaginal intercourse for 6–8 weeks
- Proper hygiene and wound care instructions
- Prompt evaluation of any vaginal discharge or bleeding
Prognosis and Long-Term Outcomes
With early detection and aggressive treatment, the prognosis for patients with postsurgical vaginal cuff anaerobic infections is favorable. Delays in management can lead to:
- Chronic pelvic pain
- Pelvic abscesses
- Fistula formation
- Infertility (in cases of subtotal hysterectomy or preservation of adnexa)
- Sepsis and mortality in extreme cases
Timely intervention and adherence to preventive protocols greatly reduce the risk of recurrence.
Frequently Asked Questions:
What causes anaerobic infections after vaginal cuff surgery?
Anaerobic infections occur due to the introduction of bacteria from the lower genital tract during surgery, particularly when mucosal integrity is compromised.
How long after hysterectomy can vaginal cuff infections occur?
Most cases present within 2 weeks postoperatively, but infections may manifest up to 30 days after surgery.
What are the signs of a vaginal cuff abscess?
Signs include pelvic pain, purulent discharge, fever, leukocytosis, and a tender or fluctuant mass on pelvic examination.
Can vaginal cuff infections be prevented?
Yes. Proper surgical technique, preoperative antiseptic protocols, and postoperative care reduce infection risk significantly.
Is hospitalization always required for treatment?
Mild cases may be managed outpatient with oral antibiotics, but moderate to severe infections often require IV therapy and possible hospitalization.
Postsurgical vaginal cuff anaerobic infections, though relatively rare, pose a serious threat to postoperative recovery and long-term pelvic health. A clear understanding of the risk factors, prompt diagnostic evaluation, and appropriate therapeutic response are essential in mitigating complications. Through meticulous surgical technique, robust infection prevention protocols, and patient education, we can ensure improved surgical outcomes and enhanced quality of care for patients undergoing gynecologic procedures.